On May 20, 2022, I received a letter from University of Cape Coast, Ghana, hich began thus:
“Dear Sir, INVITATION TO SPECIAL AWARD CEREMONY AND LAUNCHING OF 2023-2027 UCC RESEARCH AGENDA AND UCC AT 60 INVOCATION REPORT
“The Times Higher Education 2022 World Universities Ranking adjudjed University of Cape Coast (UCC) as first in Ghana and West Africa, fourth in Africa and ranked first globally for citations. This great achievement of the University was made possible by dint of your scholarly contributions and commitment to the mission of the University.
“In showing appreciation, University Management has scheduled a special ceremony to award you for your invaluable support to the course of this institution … …”
MY CONTRIBUTION THROUGH BMJ FREQUENTLY CITED
My Acceptance Speech https://youtu.be/SewHhUBEkTo after being honoured on May 31 in Ghana included the great role BMJ played in my being more cited than any other to make “The Times Higher Education 2022 World Universities Ranking place University of Cape Coast where I am Kwegyir Aggrey Professor of Human Genetics “first globally for citations”.
EDUCATION comprises correcting errors as well as proclaiming new things and emphasizing important facts. I would like to think since 1965 when BMJ published three new things for me the five Editors in succession have enabled me to correct errors, challenge received wisdom, and even make known one invention (MPSI) I made in Clinical Genetics. How these Editors have helped me publications-wise is described here. Perhaps some aspects may help doctors half my age because some of what might be called “Minor Communications” contained such not-known-about-before information that they appeared in the CITATIONS.
My profound gratitude goes to Dr Hugh Clegg, Dr Martin Ware, Dr Stephen Lock, Dr David Smith, Dr Fiona Godlee, all who were very helpful to me in the past 59 years.
WITH EDITORS DR HUGH CLEGG 1963 TO DR FIONA GODLEE TILL 2021
My detailed publications, minor and major, reflect why some continue to be cited decades after they originally appeared.
DR HUGH CLEGG 12th BMJ Editor 1947 to 1965: My first BMJ Communication was 18 June 1963 [1a]. In 1965 Dr Clegg published my “Varicose veins in pregnancy” [1b]; Torrential epistasis associated with symmetrical facial skin ulceration in sickle cell anaemia” [1c]; Colleagues and I from London’s Royal Free Hospital described “peripheral neuropathy from dialysis in end-stage renal failure” [1d]
DR MARTIN WARE The 13th BMJ Editor (1966-1975) published for me January 27, 1966 [2a]. Year 1969 was when he invited me to write “PERSONAL VIEWS” and paid me £100 for each, equivalent to 3 times my monthly Ghanaian Physician Specialist salary.
I wrote three: (i) Superstition and Phenomena in Africa [2b] (ii) Genetic Counselling in Sickle Cell Disease [2c], (iii) in 1975 he published my PERSONAL VIEW “Tafracher” the Ghanaian vital devulgarizing word [2d] https://bit.ly/3mJBMfm
Two Medical Memoranda in 1969, Ghanaian Family of 14 and 15 with not a single Normal Haemoglobin gene [2e 2f] continue to be quoted today 53 years later. Then in 1970 came “Haemolytic anaemia in pregnancy in Nigerians” [2g] and in 1971 “Malaria and Sickle cell disease” [2h].
In 1972 Dr Martin Ware rang me in Ghana to discuss an article three British doctors published with erroneous information, and which he later made the authors withdraw. He published my reactions to the authors’ article [2i 2j]. FULL MARKS to him for pursuing authors for truth. Another communication came on 28 October 1972 correcting dangerously wrong detection of sickle haemoglobin S, cited last month 50 years later [2k].
DR STEPHEN LOCK CBE 14th BMJ Editor (1975-1991) had dealings with me when AIDS was raging. In those days, articles submitted, refereed, editors’ decision, and publication took ages. But when I submitted my detailed fact-findings soon after a 6-weeks’ tour of several African countries to study grassroots epidemiology of AIDS it took just 18 days from submission date for Dr Stephen Lock to publish my “Clinical Epidemiology, not sero-epidemiology, is the answer to Africa’s AIDS Problem” [3a].
Reprint requests poured in from everywhere, 567 in all because what I described happening on my Continent was entirely different from the Media Mantra “Scientists blame African Green Monkey for AIDS in Africa, therefore Wear Condoms!” http://www.bmj.com/cgi/reprint/294/6587/1593.pdf [3a]
Dr Stephen Lock did make my voice heard not a few times 1977 [3b], 1980 [3c 3d – MPSI],1981 [3e], 1982 [3f – Sickle cell disease survey], 1984 [3g – Ethical issues in prenatal diagnosis July 21], 1985 [3h Ethnic minorities and sickle cell disease, 3i – Tribute to Prof. Hermann Lehmann], 1986 [3j – Epidemiology Correctly Defined] 1991 [3k Kwashiorkor Ghanaian tribal word origin, 3l – Penicillin prophylaxis in sickle cell disease, 3m – Morphine queried for sickle cell disease patients] – all these appear in my 434 minor and major Publications listed on www.konotey-ahulu.com or www.sicklecell.md [3n]
But what I cherished most was when Dr Lock in 2001 published the Genetic Index I invented, “MPSI”, which proved mathematically that procreation-wise females can never be the equal of males [3d].
Funny enough, Dr Stephen Lock’s last year as Editor was when I met the elegant lady who later became BMJ Editor, Dr Fiona Godlee. I had gone to BMA House to donate copy of my newly published Magnus Opus “THE SICKLE CELL DISEASE PATIENT” [3o 3p] to the Editor as I had just done to Lancet’s Editor [3q]. It was to her I gave the book to pass on to Dr Stephen Lock who was glad to see me because we both had learnt much from Professor Hermann Lehmann MD FRS in Cambridge.
DR RICHARD SMITH 15th BMJ Editor 1991-2004 published my Tribute [4a] to the remarkable Professor Dame Sheila Sherlock, the then Liver Queen of the world who with the recommendation of her husband Dr Geraint James MA MD FRCP, Teacher for the MRCP Exam of Therapeutics at Royal Postgraduate Medical School Hammersmith Hospital for the MRCP Exam, made me Research Fellow in her Department of Medicine at the Royal Free Hospital to work on the Renal Unit of the kidney giant Dr Stanley Shaldon MA MD FRCP in 1964-1965. Outcome of my research was one of the 1965 BMJ articles still quoted in 2022 on dialysis for end-stage renal failure. [1d]
Dr Richard Smith also published for me four clinical experiences for which I coined the word supra-scientific, for so each of them was, and still are. [4b].
A remarkable article by Didier Fassin and Helen Schneider [4c] revealing scientific misbehaviour in South Africa as contributing to AIDS havoc in the Black Population prompted me to respond with a 7,000-word article and 70 References which Editor Richard Smith did not reject, but published on line in its entirety [4d], available on http://www.rethinking.org/bmj/response_30917.html even today. I was 30th of 835 Responders from the year 2003 to 2005 when Dr Smith handed the Editor’s baton to Dr Fiona Godlee.
ENTERS DR FIONA GODLEE [16th BMJ Editor 2005-2021]
As soon as Dr Godlee assumed reins of the BMJ she stopped all Rapid Responses on AIDS in South Africa. I was crest-fallen because Responders had been inching nearer and nearer to what Leonard G Horowitz brilliantly dissected in 598 pages of his “Emerging Viruses: AIDS & Ebola – Nature, Accident or Intentional?” [5a].
The Didier Fassin/Helen Schneider bombshell [4c] was full of Facts authenticated by Archbishop Desmond Tutu’s Reconciliation Exercise [5b] when scientists with Nazi proclivities confessed to wrongdoing. To halt Debate on an article that revealed “Parliamentarians rejoicing at how Blacks are dying from AIDS” [4a] caused Africans to mutter “Do we now have a Racist BMJ Editor?” But Dr Fiona Godlee was not at all racist. Two years on one Debate which could go on and on indefinitely? As former Editor of Ghana Medical Journal [5c 5d 5e 5f] I have admired the way Dr Fiona Godlee has navigated choppy journalistic waters. Paranoid African spectacles make me sometimes impatient with what I read in the BMJ, but as I put myself in her shoes, I admit freely she had done much better than I would have ever done. I gave her “Pluses” for making my voice heard very often in BMJ-on-line as indicated below:
ONE AFRICAN DOCTOR’S TESTIMONY TO DR FIONA GODLEE’S KINDNESS
I said EDUCATION involves correcting misinformation, teaching new things, underlining irrefutable facts, and challenging Received Wisdom.
“Kwashiorkor” – name we in my Krobo-Dangme-Ga mega tribe in Ghana [5g] have for centuries had for the childhood disease later described by Cicely Williams [5h 5i] – was the first article [224 in Publications List] of some 100 times in the BMJ that the Editor Dr Godlee permitted my voice to be heard from 14 May 2005 to 2021.
Researchers who cited me freely agree that the “List of Publications” found in www.konotey-ahulu.com or www.sicklecell.md [3j] reveals where Misinformation apart from that of Kwashiorkor in textbooks has been corrected.
For example, there has been widespread misinformation that sickle cells protect against malaria, when in fact malaria is known to be the greatest killer of children with sickle cell disease in Africa [3a 5k(284) 5l 5m].
I was born of Trait parents into a Sickle Cell Disease home with 3 sickle cell disease children of 11 offspring, enabling me as a doctor to place “The Sickle Cell Disease Patient” above “Sickle Cell Disease”. Malaria always brought on sickle cell crisis! To allow patients’ wellbeing, “Clinical Experience” which was with me from childhood was enhanced as a doctor to value it above “Haematological Experience” [5n].
Supernatural Phenomena, Darwinian Evolution, Public Health including Vaccinology form part of my publications list.
Dr Fiona Godlee continued to make my voice heard on several different topics allowing me to challenge Received Wisdom: Using my Publications List references to check, other articles are Human resources for health in Africa [234], Doctors as lapdogs to drug firms [260], Prenatal tests and abortion [261 331 334 417], Traditional Medicine [262], Stethoscope and Parkinson’s Kap’s sign [264 295], Sickle Cell Care centres [266], Four bodyguards for speaking scientific truth [271], Pharmacovigilance [272], Opiates for dying and sickle cell disease patients [273], Circumcision and alleged AIDS protection [275], Malaria [279 302 304 320], UK Sickle Cell Disease Patient mismanagement [280 293], Vaccines for genital warts [285], International Donors and conflicting interests [286 293], Conflicting Advice in Clinical Medicine [287 316], Haemodialysis, home and other [ 288 291 315], The soul is supra-scientific [294], NCEPOD Report Poor care of sickle cell disease patients in UK [296 300 357], Sickle Cell Disease Patient management [374 419], Internet Revolution [301], BMJ Archive and other [303 360], Genetic Testing HGC and Public Health [305 408], Blowing own trumpet [306], Fixed drug eruption [307
310], Abdominal aortic aneurysm [309], Free health care must demand responsibilities [311], Drug related deaths rising, and NICE [313 357 358], Honest nurses [314], Politics and Science [317], G6PD Deficiency [321], Genetic Code is supra-scientific [322], Editors and Peer review [324], Modern Genetics blind alley? [327], WHO and H1N1 Pandemic [329], Pain relief politics and economics [330], President Obama apologises over unethical Guatemala syphilis study [332], Nobel Laureate Robert Edwards [333], Physician Dr Geraint James [336], Ethics of gene replacement [337], Music and Tonal Language [339 340], Evangelical Christian appointment controversy [342], Scientific African Revolution through Facebook and Twitter [343], Belief in God ridiculed [301 344 345 346 399], Epistaxis [353], Wikipedia [356], NHS Hospital Delivery Care questioned [358], Pulmonary embolism [361 364], Liverpool Care and Assisted Dying [362 365], Clinical Guidance in Chemotherapy [367], Opiods in the UK [368], Osteomyelitis [370], Erectile Dysfunction [371], Ebola and HIV AIDS [384 385 386], Medical Ethics: Scientists abandon moratorium on germ line editing [387], Sickle cell hip pathology [388 421], Home Office VISA [391 392], Brexit and Democracy [393], International Medical Graduates and quality of care [401], Routine blood tests [403], International fraud and drugs [406], GOD mentioned in BMJ Editorial [409 410], Personal Faith [411], Aviation safety and scientific misinformation [418], Evidence, the human dimension [423], Transgenderism [424 424a], COVID-19 [427 428 429 432].
Is all this part of the reason almost every week, ACADEMIA (Oxford) and ResearchGate (Berlin) alert me that they have observed someone, somewhere, somewhen, has cited me in their publications?
It seems to me the only Minus I observed from Dr Fiona Godlee in a multitude of Pluses was when she allowed that tail-wagging-the-dog Editorial which suggested we replace sex-at-birth with gender later-on [424a]. Sharing in her huge success, I must mention Dr Kamran Abbasi (now Editor), Dr Peter Doshi, and Ms Sharon Davies. Well Done, Great Team, and Thank You!
CONCLUSIVE REMARKS
1. Personal interactions in the past of an aged physician like myself (92 years on 12th July 2022) with a world class Medical Journal like the BMJ may well help in one way or other Consultants half my age, Registrars a third my age, House Officers quarter my age.
2. Tribal Information on Kwashiorkor, and Sickle Cell Disease Patients with Malaria, can expose scientific misinformation.
3. Received Wisdom must not just be accepted because it is trumpeted by so-called experts and accredited Committees and Organisations like WHO, NICE, and NIH..
4. It needs to be proclaimed to students and teachers that Science cannot be used by anybody however brilliant to explain everything.
5. That Science has no place for GOD has not prevented BMJ editorials on GOD.
6. Ethics is not part of science because lying scientists and scientific liars exist.
7. Editorial Integrity decade after decade has placed the BMJ top of the global Class.
8. Personal gratitude to the BMJ requires acknowledgement.
Conflict of Interest: None Declared, but Bias stems from longevity by the grace of GOD which has made my very first ever major article published in 1965 [Sicklaemic Human Hygrometers, Lancet 1965; 1: 103-104] cited in June and October 2022]
felix@konotey-ahulu.com Twitter@profkonoteyahul
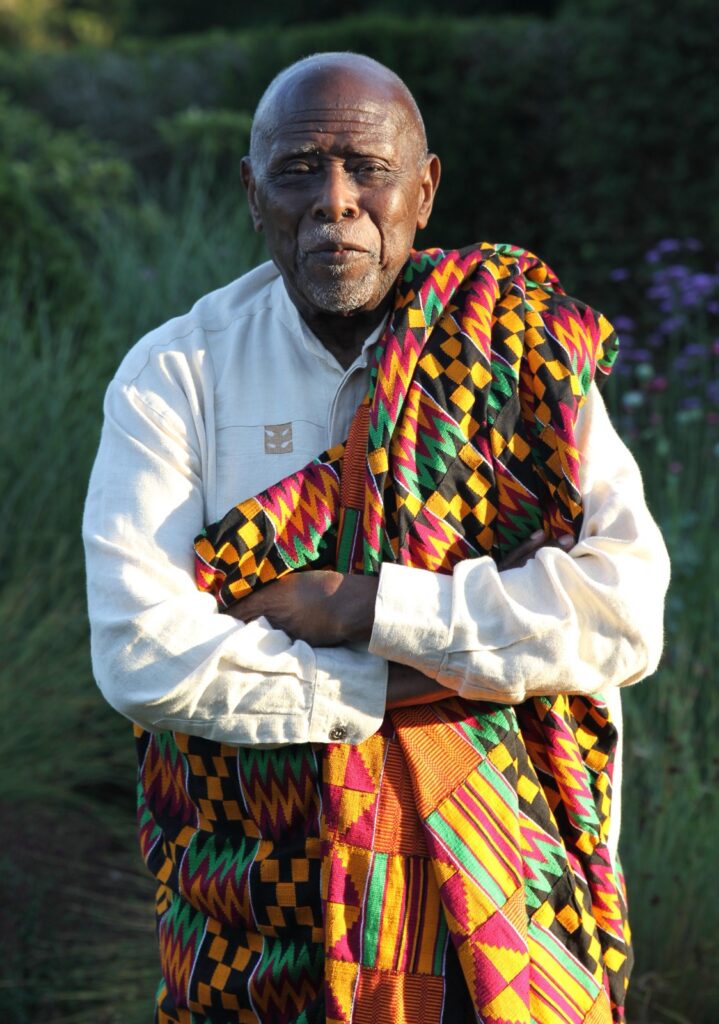
Felix I D Konotey-Ahulu FGA MB BS MD(Lond) DSc(UCC) DSc(UH) FRCP(Lond) FRCP(Glasg) DTMH(L’pool) FGCP FWACP FTWAS ORDER OF THE VOLTA (OFFICER) Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast, Ghana; Former Consultant Physician Genetic Counsellor in Sickle Cell and Other Haemoglobinopathies Korle Bu Teaching Hospital & Director Ghana Institute of Clinical Genetics and at Cromwell Hospital London SW5 0TU, and 9 Harley Street, Phoenix Hospital Group, London W1G 9AL [www.sicklecell.md] https://youtu.be/41a1FZSpHd4 & https://youtu.be/SevUBEHhTo for Awards on video]
References
1a Konotey-Ahulu FID. “Case of lightning burns” BMJ 1963; 1: 1547. June 18 1963 doi:10.1136/bmj.1.5344.1547 http://www.bmj.com/cgi/reprint/1/5344/1547-apdf
1b Konotey-Ahulu FID. Varicose veins in pregnancy. BMJ 1965; 2: 1065. doi:10.1136/bmj.2.5469.1065 www.bmj.com/cgi/reprint/25469/1065.pdf
1c Konotey-Ahulu FID. Torrential epistaxis associated with symmetrical facial skin ulceration in sickle cell anaemia. BMJ 1965 Oct; 2: 859-860. doi:10.1136/bmj.2.5466.859 http://www.bmj.com/cgi/reprint/2/5466/859.pdf
1d Konotey-Ahulu FID, Baillod RA, Comty CM, Heron JR, Shaldon S, Thomas PK. Effect of periodic dialysis on the peripheral neuropathy of end-stage renal failure. BMJ 1965; 2: 1212-1215 (Nov. 20) doi:10.1136/bmj.2.5472.1212 http://www.bmj.com/cgi/reprint/2/5472/1212.pdf
2a Konotey-Ahulu FID. Epistaxis in sickle cell anaemia (12 References). BMJ 1966; 1: 234. doi:10.1136/bmj.1.5481.234-a (January 27)
2b Konotey-Ahulu FID. Personal View (Superstition and phenomena in Africa). BMJ 1969; 2: 48 doi:10.1136/bmj.2.5648.48 http://www.bmj.com/cgi/reprint/2/5648/48.pdf (April 15, 1969)
2c Konotey-Ahulu FID. Personal View (Genetic counselling in sickle-cell disease). BMJ 1969; 3: 235 doi:10.1136/bmj.3.5664.235 [Substitute ACHE for ‘bad’ and ‘wrong’, and NORM for ‘good’] http://www.bmj.com/cgi/reprint/3/5664/235.pdf
2d Konotey-Ahulu FID. Tafracher – Personal View. BMJ 1975; 1(5953): 329. (Feb. 8 doi:10.1136/bmj.1.5953.329 http://www.bmj.com/cgi/reprint/1/5953/329.pdf Ghanaian Devulgarising word https://bit.ly/3mJBMfm
2e Konotey-Ahulu FID and Ringelhann B. Sickle-cell anaemia, sickle-cell thalassaemia, sickle-cell haemoglobin C disease and asymptomatic haemoglobin C thalassaemia in one Ghanaian family. BMJ 1969 Mar 8; 1(5644): 607-612. doi:10.1136/bmj-1.5644/607 http://www.bmj.com/cgi/reprint/1/5644/607.pdf
2f Bentsi-Enchill KK, Konotey-Ahulu FID. Thirteen children from twelve pregnancies in sickle-cell thalassaemia. BMJ 1969; 3: 762 doi:10.1136/bmj.3.5673.762
2g Konotey-Ahulu FID. Haemolytic anaemia in pregnancy in Nigerians. BMJ 1970: 2(5701): 112 doi: 10.1136/bmj.2.5701.112-a (April 11)
2h Konotey-Ahulu FID. Malaria and sickle-cell disease BMJ 1971 June; 2(5763): 710-711 doi:10.1136/bmj.2/5763.710-d
2i Konotey-Ahulu FID. Sickle Cell Trait and altitude. BMJ 1972; 1(5793): 177-78 January 15 doi:10,1136/bmj.1,5793.177-a http://www.bmj.com/cgi/reprint/1/5793/177-a.pdf
2j Konotey-Ahulu FID. Sickle cell and altitude. BMJ 1972;2: 231-232. 2k Konotey-Ahulu FID. Detecting sickle haemoglobin. BMJ 1972; 4: 239.
3a Konotey-Ahulu FID. Clinical epidemiology, not sero-epidemiology, is the answer to Africa’s AIDS problem BMJ (Clin Res Ed) 1987; 294(6587): 1593-1594 (June 20 1987) doi:10.1136/bmj.294.6587.1593 http://www.bmj.com/cgi/reprint/294/6587/1593.pdf
3b Konotey-Ahulu FID. Personal View: The spiritual and the psychological in Clinical Medicine. BMJ 1977; 1: 1595. (June 15) doi:10.1136/bmj.1.6076.1595 http://www.bmj.com/cgi/reprint/1/6076/1595.pdf
3c Konotey-Ahulu FID. English-speaking peoples. (Book Review: English Tests for Doctors by Dick Alderson and Vivienne Ward). BMJ 1980; 280 May 24: 1267-1268. doi:10.1136/bmj.280.6226.1267 http://www.bmj.com/cgi/reprint/280/6226/1267.pdf
3d Konotey-Ahulu FID. Male procreative superiority index (MPSI): The missing co-efficient in African anthropogenetics. BMJ 1980; 281(6256): 1700-1702 doi:10.1136/bmj.281.6256.1700 http://www.bmj.com/cgi/reprint/281/6256/1700.pdf http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1715685&blobtype=pdf |
3e Konotey-Ahulu FID. Problems of overseas doctors. BMJ Clin Research Ed; 282(6276 :1621-1622 doi:10.1136/bmj.282.6276.1621-a http://www.bmj.com/cgi/reprint/282/6276/1621-a.pdf 1981 May 16 1981
3f Konotey-Ahulu FID. Survey of sickle-cell disease in England and Wales. http://www.bmj.com/cgi/reprint/284/6309/112-a.pdf BMJ 1982; 284(6309): 112. doi:10.1136/bmj.284/6309/112a January 9, 1982.
3g Konotey-Ahulu FID. Ethical issues in prenatal diagnosis. BMJ Clin Res Ed 1984; 289(6438): 185. July 21. doi:10.1136/bmj.289.6438.185-a 6143955 http://www.bmj.com/cgi/reprint/289/6438/185-a.pdf
3h Konotey-Ahulu FID. Ethnic minorities and Sickle Cell Disease. BMJ Clin Res Ed 1985; 290(6476): 1214 http://www.bmj.com/cgi/reprint/290/6476/1214.pdf
3i Konotey-Ahulu FID. Tribute to Professor Hermann Lehmann CBE, MD, PhD, ScD, FRCP, FRCPath, FRSC, FRS. BMJ 1985; 291: 288-289. (July 27, 1985) doi:10.1136/bmj.291.6490.288
3j Konotey-Ahulu FID. Points: A boost for clinical research. BMJ April 1986, page 1081 “If, as I have always thought, the discipline of clinical epidemiology seeks to answer the questions How? Which? When? Who? What? Why? Where? Are we more likely
to get clearer answers in the north to questions relating to the south?” http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1340158&blobtype=pdf
3k Konotey-Ahulu, FID. Kwashiorkor. BMJ 1991, 302(6769): 180-181. Jan 19. (Explaining what this Ghanaian tribal word means) doi:10.1136/bmj.302.6769.180-chttp://www.bmj.com/cgi/reprint/302/6769/180-c.pdf
3l Konotey-Ahulu, FID. Penicillin prophylaxis in children with sickle cell disease. BMJ 1991; 302(6786): 1205-06. (May 18 1991) doi:10.1136/bmj.302.6786.1205-b (Commenting on paper by Cummins, Heuschkel & Sally Davies – Brit Med J 1991; 302: 989-90.) http://www.bmj.com/cgi/reprint/302/6786/1205-b.pdf
3m Konotey-Ahulu, FID. Morphine for painful crises in sickle cell disease. BMJ 1991, 302(6792): 1604. (June 29) doi:10.1136/bmj.302.6792.1604-c http://www.bmj.com/cgi/reprint/302/6792/1604-c.pdf (Comment on Professor Chamberlain’s recommendation of morphine in pregnancy in sickle cell disease – BMJ 1991; 302: 1327-30.)
3n Konotey-Ahulu FID. Website on Sickle Cell Disease Patient www.sicklecell.md and www.konotey-ahulu.com
3o Konotey-Ahulu FID. The Sickle Cell Disease Patient. The Macmillan Press Ltd.,1991 & Reprinted 1992. Republished 1996 by T-AD Co [See 3n below]
3p Konotey-Ahulu FID. The Sickle Cell Disease Patient. TETTEH-A’DOMENO COMPANY 1996, P O Box 189, Watford WD1 7NJ, England. ISBN 0-95- 9515442-2-
5 Foreword by Professor Roland B Scott MD, Howard University Center for Sickle Cell Disease. [643 pages]
3q Weatherall Professor Sir David FRS MD FRCP FRCPath. Lancet June 29, 1991 Volume 337 page 1590 says “The Sickle Cell Disease Patient” is a fitting tribute to a physician who has done as much as anyone to improve facilities to deal with this condition in Africa.
4a Konotey-Ahulu FID. Dame Sheila Sherlock’s Third World Dimension. BMJ rr 20 Jan 2002 http://www.bmj.com/content/324/7330/174.1.extract.reply#bmj_el_18859
4b Konotey-Ahulu FID. The supra-scientific in clinical medicine: a challenge for Professor Know-All. http://www.bmj.com/cgi/reprint/323/7327/1452.pdf Brit Med J 2001; 323(7327):14521453 Dec 22-29 doi:10.1136/bmj.323.7327.1452
4c Fassin Didier, Schneider Helen. The Politics of AIDS in South Africa: beyond the controversies. BMJ 2003; 326: 495 https://doi.org/10.1136/bmj.326.7387.495 March 1 2003.
4d Konotey-Ahulu FID. Wake-up call and need for paradigm shift. Brit Med Journal 2003 ‘Rapid E-Response’ to Didier Fassin and Helen Schneider’s article opened up for Education and Debate: – The politics of AIDS in South Africa: beyond the controversies. Brit Med J 2003; 326; 495-497 (1 March 2003). [7000 words with 70 references] http://www.rethinking.org/bmj/response_30917.html
5a Horowitz Leonard G. Emerging Viruses: AIDS and Ebola – Nature, Accident or Intentional? Tetrahedron, Inc. Rockport MA, 1998 ISBN: 0-92350-12-7
5b Maharaj Akaash. Desmond Tutu was right. The Truth and Reconciliation Commission. Report submitted October 28, 1998.
5c Konotey-Ahulu FID. Toxoplasmosis. Ghana Medical Journal 1970; 9: 67-68 (Editorial – 7 references)
5d Konotey-Ahulu FID. Vitamin A in Cholesterol biosynthesis and pathogenesis of atherosclerosis (Editorial) Ghana Medical Journal 1972; 11: 3-4.
5e Konotey-Ahulu FID. An International Sickle Cell Crisis. Ghana Medical Journal March 1972; 11: 4-8 (Editorial)
5f Konotey-Ahulu FID. The Tyranny of Fashion in Medical Journals. Ghana Medical Journal [Editorial], 1972; 11: 168-172.
5g Konotey-Ahulu FID. Issues in Kwashiorkor. Lancet 1994 February 26, Volume 343, page 548. [Lancet published picture of Dr Cicely Williams and me in Oxford at Somerville College when I accompanied Ghana High Commissioner His Excellency Annan Cato and Vice Chancellor University of Ghana Professor Akilagpa Sawyerr to confer Honorary DSc on the remarkable lady who first described Kwashiorkor using the Krobo-Dãngme-Gã Tribal word for the malady in the world Medical Journals. Correcting widespread misinformation about what my tribal name Kwashiorkor means I said in this Lancet communication “Kwashiorkor is the result of a social Pathology before it is outcome of a biochemical pathology”. It does not mean red hair!
5h “Mechanism through which Hb S protects against malaria” on pages 94, 95, 96 of Konotey-Ahulu FID The Sickle Cell Disease Patient. The Macmillan Press Ltd.,1991 & Reprinted 1992. Republished 1996 by T-AD Co [See comment on page 94 last paragraph: “One obvious puzzling question is why sickle cell homozygotes do not show the same clinical resistance to falciparum malaria as sickle cell Traits.
5i Konotey-Ahulu FID. The Sickle Cell Diseases: Clinical Manifestations including The Sickle Crisis. Archives Internal Medicine 1974; 133; 611-619. [Comprehensive]
5j Konotey-Ahulu FID. Effect of environment on sickle cell disease Environment in West Africa: epidemiological and clinical considerations. In Sickle Cell Disease. Diagnosis, management, education, and research. Abraham H et al. C V Mosby o, St Louis, pages 20-38.
224 Konotey-Ahulu FID There is nothing mysterious about Kwashiorkor. BMJ 14 May 2005 Rapid Response http://www.bmj.com/cgi/eletters/330/7500/1095#106854
234 Konotey-Ahulu FID Human resources for health in Africa. Is it national or international policies causing the brain drain? BMJ Rapid Response November 7 to Editorial by Adetokunba O Lucas “Health resources for health in Africa” BMJ 2005, 331: 1037-1038 http://www.bmj.com/cgi/eletters/331/7524/1037#120815
260 Konotey-Ahulu FID. Doctors must not be lapdogs to drug firms even more relevant in the Third World. BMJ Rapid Resp. November 12 2006 http://www.bmj.com/cgi/eletters/333/7576/1027#149040
261 Konotey-Ahulu FID. Refusing to provide a prenatal test for reducing later termination of pregnancy can it ever be ethical? BMJ
http://www.bmj.com/cgi/eletters/333/7577/1066#149662 BMJ Rapid Resp. Nov. 20, 2006
262 Konotey-Ahulu FID Recovering lost knowledge of traditional medicine by searching historical herbal texts for potential new drugs. http://www.bmj.com/cgi/eletters/333/7582/1314#152179 BMJ Rapid Resp. Dec. 26, 2006
264 Konotey-Ahulu FID My stethoscope’s bell and discovery of a new Parkinsonian physical sign (Kap’s sign) in clinical medicine, BMJ Rapid Response 6 Feb 2007.
http://www.bmj.com/cgi/eletters/334/7587/253#157649
266 Konotey-Ahulu FID. Dedicated sickle cell centres. BMJ Rapid Response March 20, 2007 http://www.bmj.com/cgi/eletters/334/7591/477#
271 Konotey-Ahulu FID. Four bodyguards and the perils of unmasking scientific truths. BMJ 2007; 335: 210-211 July 28, 2007.
.http://www.bmj.com/cgi/content/full/335/7612/210
http://www.bmj.com/cgi/reprint/335/7612/210.pdf
272 Konotey-Ahulu FID. Who should best pharmacovigilate in developing countries? 14 September 2007 http://www.bmj.com/cgi/eletters/335/7618/462#167455 Rap Resp to Editorial
273 Konotey-Ahulu FID. Opiates for pain in dying patients and in those with sickle cell disease. 11 October 2007 BMJ Rapid Resp. http://www.bmj.com/cgi/eletters/335/7622/685#177986
275 Konotey-Ahulu FID Male circumcision and alleged protection from AIDS. BMJ Rapid Response (Dec. 11) http://www.bmj.com/cgi/eletters/335/7631/1206#183100
276 Konotey-Ahulu FID. Ghana @ 50 UK Health Conference: A special report. Ghanaian Times Dec. 24, 2007, p. 24.
279 Konotey-Ahulu FID. Imported malaria in the UK: Unde venis? & Quo vadis?
http://www.bmj.com/cgi/eletters/337/jul03_2/a135#198874 BMJ Rap Resp 16 July 2008
280 Konotey-Ahulu FID. Current “hit and miss” care provision for sickle cell disease patients in the UK http://www.bmj.com/cgi/eletters/337/jul11_2/a771#199135 BMJ Rapid Resp. 22 July 2008
283 Konotey-Ahulu FID. Management of sickle cell disease versus management of the sickle cell disease patient. BMJ Rapid Resp.17 September 2008
http://www.bmj.com/cgi/elettrs/337/sep08_1/a1397#202088
284 Konotey-Ahulu FI D. Malaria and sickle cell: “Protection?” Or “No Protection?” – Confusion reigns. BMJ Rapid Response October 13 2008
http://www.bmj.com/cgi/eletters/337/oct01_3/a1875#203067
285 Konotey-Ahulu FID. Vaccination for genital warts to prevent cervical cancer: principles first, please, before details. BMJ Rapid November 12 2008 http://www.bmj.com/cgi/eletters/337/oct23_1/a2186#204534
286 Konotey-Ahulu FID. Affordable Antimalarials: Do international Donors not have conflicting interests? BMJ Rapid Response November 25, 2008 http://www.bmj.com/cgi/eletters/337/nov12_1/a2495#205142
287 Konotey-Ahulu FID. Clinicians facing conflicting recommendations: Use common sense? http://www.bmj.com/cgi/eletters/337/nov28_2/a2530#205677 BMJ Rapid Resp. Dec. 5, 2008.
288 Konotey-Ahulu FID. Home haemodialysis just the thing for Africa’s wealthy patients. http://www.bmj.com/cgi/eletters/336/7634/3#186073 BMJ Rapid Response 8 January 2008
291 Konotey-Ahulu FID. But how much does maintenance haemodialysis cost in each country? BMJ Rapid Resp. 31 January 2008 http://www.bmj.com/cgi/eletters/336/7634/3#188633
292 Konotey-Ahulu FID. Domiciliary management is the way forward for AIDS management in Africa. [March 4 2008] Comment on “Reduced mortality with home-based HIV treatment in Uganda” Comment – Lancet 2008; 371: 703-705
293 Konotey-Ahulu FID. Do international donors genuinely desire to help solve Africa’s health problems? BMJ Rap Resp. 19 March 2008 http://www.bmj.com/cgi/eletters/336/7643/518#192285
294 Konotey-Ahulu FID. The soul is supra-scientific. BMJ Rapid Response 16 May 2008.http://www.bmj.com/cgi/eletters/336/7653/1132#195557
295 Konotey-Ahulu FID. The stethoscope is there for life and will remain for good. http://www.bmj.com./cgi/eletters/336/7653/1134#195928 BMJ Rapid Response May 28, 2008.
296 Konotey-Ahulu FID. Poor care for sickle cell disease patients: This wake-up call is overdue. BMJ Rapid Response May 28, 2008 BMJ 2008; 336: 1152 to Susan Mayor “Enquiry shows poor care for patients with sickle cell disease” on National Confidential Enquiry into Patient Outcome and Death (NCEPOD) REPORT “SICKLE: A Sickle Crisis? (2008) http://www.bmj.com/cgi/eletters/336/7654/1152a#196224 | http://www.info@ncepod.org http://www.ncepod.org
300 Konotey-Ahulu FID. Inquest into diamorphine deaths: Does NCEPOD sickle patients report warrant a similar inquest? http://www.bmj.com/cgi/eletters/338/mar03_3/b903#210208 BMJ Rapid Response March 7 2009
301 Konotey-Ahulu FID. Martin Luther’s Protestant Reformation as a retrospective mirror for the present Internet Revolution. BMJ Rapid Response March 25, 2009
http://www.bmj.com/cgi/eletters/338/mar18_1/b1080#211184
302 Konotey-Ahulu FID. Fighting Malaria: Isn’t the best approach through Environmental Hygiene and Public Health? http://www.bmj.com/cgi/eletters/338/apr20_2/b1627#212782 BMJ Rapid Response April 26 2009
303 Konotey-Ahulu FID. British Medical Journal Archive since 1840. http://www.bmj.com/cgi/eletters/338/apr29_1/b1744#213088 BMJ Rapid Response May 2 2009.
304 Konotey-Ahulu FID. Combating malaria: Try public health measures in Africa too. BMJ 2009; 338:b 1971 doi:10.1136/bmj.b1971 (May 20) PMID: 19457959
BMJ Rapid Response 27 June 2009
305 Konotey-Ahulu FID. Human Genetics Commission (HGC) and direct to consumer Genetic Tests, leading to Genetic Counselling. BMJ Rap Resp. May 27, 2009. http://www.bmj.com/cgi/eletters/338/may15_2/b1995#214256
306 Konotey-Ahulu FID. Blow your own trumpet and be thoroughly scriptural.
http://www.bmj.com/cgi/eletters/338/june23_3/b2409#215860
307 Konotey-Ahulu FID. Fixed drug eruption with Paracetamol. BMJ Rap resp. to Charles Quartey-Papafio in BMJ 2009; 338: b2582 http://www.bmj.com/cgi/eletters/338/jun30_2/b2582#216215
309 Konotey-Ahulu FID. Abdominal aortic aneurysm screening for men: Please acknowledge a genetic dimension http://www.bmj.com/cgi/eletters/338/jun24-_2/b2307#216519 BMJ 10 July 2009
310 Konotey-Ahulu FID. Fixed drug eruptions. More of fixed rug eruptions. http://www.bmj.com/cgi/content/full/bmj.b2924
311 Konotey-Ahulu FID. Free health care for world’s poorest countries without pre-conditions? BMJ Rapid response Aug 7 [In response to Zosia Kmietowicz http://www.bmj.comcgi/eletters/339/aug05_1/b3177#218219 | http://www.bmj.com/cgi/content/full/339/aug05_1/b3177 BMJ 2009;339.b3177
313 Konotey-Ahulu FID. UK drug related deaths are still rising: So where is NICE? Sept. 6 2009 http://www.bmj.com/cgi/eletters/339/sep01_1/b3536#219836
BMJ Rapid Response to Susan Mayor on “UK drug related deaths are still rising 2 reports say” .
314 Konotey-Ahulu FID. Doctor cleared of asking nurse to give fatal dose to dying patient: More honest nurses, please 17 Sept. BMJ 2009; 339: b3812
http://www.bmj.com/cgi/eletters/339/sep15_3/b3812#220512
315 Konotey-Ahulu FID. High index of suspicion with timely haemodialysis for hyperkalaemic cardiac arrest. Rapid Resp.5 Nov 2009.
http://www.bmj.com/cgi/eletters/339/oct23_1/b4114#224409 .
316 Konotey-Ahulu FID. Does rejecting a particular scientific opinion mean a rejection of science? http://www.bmj.com/cgi/eletters/339/nov04_1/b4563#224533 Rapid Resp.10 Nov. 2009.
317 Konotey-Ahulu FID. Harold Varmus and The Art of Politics and Science. http://www.bmj.com/cgi/eletters/339/nov17_3/b4848#225563 BMJ Rapid Response 20 November 2009
321 Konotey-Ahulu FID. Are patients with G6PD Deficiency to avoid eating prawns http://www.bmj.com/cgi/eletters/340/feb26_1/c1016#232266
323 Konotey-Ahulu FID. Malaria diagnosis and treatment in Ghana. BMJ Rapid Response 25 March 2010 http://www.bmj.com/cgi/eletters/340/mar05_1/c930#233389
324 Konotey-Ahulu FID. Peer review, yes, but good editors must have the last word. http://www.bmj.com/cgi/eletters/340/mar15_1/c1409#233845 BMJ Rapid Response April 2 2010
327 Konotey-Ahulu FID. Is modern genetics a blind alley? Not quite so in Europe, but probably yes i Africa http://www.bmj.com/rapid.response/2011/1102/modern-genetics-blind-alley-not-quite-so-europe-probably-yes-africa BMJ Rapid Response 19 May 2010
329 Konotey-Ahulu FID. WHO declares that H1N1 Pandemic is officially over: So do Ghanaians need to be jabbed with the vaccine? BMJ 12 Aug 2010 Rapid Resp.
http://www.bmj.com/cgi/eletters/341/aug11_c4393#240213
330 Konotey-Ahulu FID. The politics (and economics) of pain relief in the West and Third World. 24 August 2010 BMJ Rapid Response to T Anderson http://www.bmj.com/cgi/eletters/341/aug11_2/c3800#240684 The politics of pain 11 Aug doi: 10.1136/bmj.c3800
331 Konotey-Ahulu FID. Antenatal screening for sickle cell disease and beta-thalassaemia. http://www.bmj.com/content/341/bmj.c5132/reply#bmj_el_242914 BMJ Rapid Response Oct 12 2010 [32 references]
332 Konotey-Ahulu FID. President Obama apologises over Guatemala syphilis study: International cooperative research in jeopardy. BMJ Rapid response October 17 2010. [16 references] http://www.bmj.com/content/341/bmj.c5494.full/reply#bmj_el_243183
333 Konotey-Ahulu FID. Genius of Nobel Laureate Robert Edwards goes beyond IVF. http://www.bmj.com/content/341/bmj.c5533/reply#bmj_el_243005 | www.embryologist.org.uk BMJ Rapid Response Oct 14 2010 [3 references]
334 Konotey-Ahulu FID. Antenatal sickle cell disease haemoglobinopathy screening.
http://www.bmj.com/content/341/bmj.c5243/reply#bmj_el_243447 BMJ Rapid Respo Oct. 25, 2010
336 Konotey-Ahulu FID. David Geraint James: Great Champion of Overseas Postgraduates. 18 Nov 2010 [Resp. to BMJ 341:doi.1136/bmj.c6400] See Ref 170 on Dame Sheila Sherlock 20 Jan 2002 http://www.bmj.com/content/341/bmj.c6400.full/reply#bmj_el_244903 | http://www.bmj.com/content/324/7330/174.1.extract.reply#bmj_el_18859
337 Konotey-Ahulu FID. Ethics of mitochondrial gene replacement is also ethics of acquired genetic inheritance. BMJ Rapid Response 19 November 2010
http://www.bmj.com/content/341/bmj.c6021/full/reply#bmj_el_244910
339 Konotey-Ahulu FID. Music (and Tonal Language) and the art of being human http://www.bmj.com/content/341/bmj.c6965.full/reply#bmj_el_246612 BMJ Rapid Response Dec 20.
340 Konotey-Ahulu FID. Music (and Tonal Language) and the art of being human II. http://www.bmj.com/content/341/bmj.c6965.full/reply#bmj_el_246615 BMJ Rapid Response Dec 20.
341 Konotey-Ahulu FID. Music (and Tonal Language) and the art of being human III. http://www.bmj.com/content/341/bmj.c6965.full/reply#bmj_el_246618. BMJ Rapid Response Dec 20.
342 “New appointment of evangelical Christian to drug advisory body sparks controversy” Please spare us emotive headlines BMJ Rapid Response 6 February 2011 http://www.bmj.com/content/342/bmj.d624/reply#bmj_el_249481
343 Konotey-Ahulu FID. Facebook and Twitter in bid to create African Scientific Revolution “mizraimically” BMJ paid Response 5 March 2011
.http://www.bmj.com/content/342/bmj.d948/reply#bmj_el_251007
344 Konotey-Ahulu FID Only fruitcakes believe in GOD? http://www.bmj.com/content/342/bmj.d2642/reply#bmj._el_260425
[See Correction in Reference 301] BMJ Raid Response 11 May 2011.
345 Konotey-Ahulu FID. Only fruitcakes believe in in GOD? Correction of inverted inheritance of solomonic genius. BMJ Rapid Response 12 May2011. [See Reference 300] http://www.bmj.com/content/342/bmj.d2642/reply#bmj_el_260496 BMJ Rapid Response 12 May2011. [See Reference 300]
346 Konotey-Ahulu FID. Is talking about God to be banned from clinical care? http://www.bmj.com/content/342/bmj.d3275/reply#bmj_el_261475 BMJ Rapid Resp. 2 June 2011.
353 Konotey-Ahulu FID. Epistaxis from sickle cell disease must not be forgotten www.bmj.com/content/344/bmj.e1097/rr/576087 BMJ Rapid Response 28 March 2012
356 Konotey-Ahulu FID. Should clinicians edit Wikipedia to engage a wider world web? At least two examples of inaccuracy dictate caution BMJ 14 August 2012 Rapid Response www.bmj.com/content/345/bmj.e4275/rr/598116
357 Konotey-Ahulu FID. Management of an acute painful sickle cell episode in hospital: NICE guidance is frightening1 Sept 7, 2012. www.bmj.com/content/344/bmj.e4063/rr/599158 [42 references]
358 Konotey-Ahulu FID. Almost a quarter of Royal College Fellows say their hospitals cannot deliver continuity care. And they boast of something called National Institute of Clinical Excellence? www.bmj.com/content/345/bmj.e4942/rr/601191 September 7, 2012 BMJ Rapid Response.
360 Konotey-Ahulu FID Bring back good quality paper in the print BMJ www.bmj.com/content/345/bmj.e6396/rr/610395 BMJ Rapid Response 23 October 2012
361 Konotey-Ahulu FID. Diagnosis and management of pulmonary embolism. www.bmj.com/content/346/bmj.f767/rr/633072 BMJ Rapid Response 26 Feb 2013
362 Konotey-Ahulu FID. Liverpool care pathway BMJ and Channel Four News: Majority expert choice does not mean best choice March 8 2013 BMJ Rapid Response to “Nine out of 10 palliative care experts would choose Liverpool care pathway for themselves” Krishna Chinthapalli BMJ 2013; 346: 1103 (March 2, pages 2-3) www.bmj.com/content/346/bmj.f1303/rr/634971
364 Konotey-Ahulu FID. Importance of history in the diagnosis of pulmonary embolism www.bmj.com/content/346/bmj.f1692 March 19 BMJ 2013; 366: F1692
365 Most religious followers support assisted suicide for the dying: Survey flawed through inadequate definition of “religious” and “terminally ill”. BMJ Rapid Response May 12 2013 www.bmj.com/content/346/bmj.f2855/rr/645095 – to Zosia Kmietowicz BMJ News www.bmj.com/content/346/bmj.f28555?sso 11 May: Most religious followers support assisted suicide for the dying.
367 Konotey-Ahulu FID. Opiods for chronic non-cancer pain – Chemotherapy – Clinical Guidelines: Where does ultimate responsibility lie? www.bmj.com/content/ 346/bmj.f2937/rr/651421 BMJ Rapid Response 25 June 2013
368 Konotey-Ahulu FID. Opiods in the UK: What’s the problem? Answer – Good Clinical Practice needs to cover all population groups including sickle cell disease patients. www.bmj.com/content/347/bmj.15108/rr/658208 BMJ Rapid Response 18 August 2013
370 Konotey-Ahulu FID. Acute osteomyelitis in African children unmasks sickle cell disease with salmonellosis http://www.bmj.com/content/348/bmj.g66/rapid-responses BMJ Rapid Response Feb. 1, 2014
371 Konotey-Ahulu FID. Erectile Dysfunction: Test, please, for Sickle Cell Disease. http://www.bmj.com/content/348/bmj.g129/rapid-responses Rapid Response to BMJ 2014; 348: g129 February 1,3 2014
374 Konotey-Ahulu FID. Management of sickle cell disease patient I the community BMJ Rapid Response 13 April 2014 [90 References] to Brousse V, Makali J, Rees DC: Management of sickle cell disease in the community. BMJ 2014; 348: g1765 doi:10.1136/bmj.g1765 http://www.bmj.com/content/348/bmj.g1765/rr/694233
378 Konotey-Ahulu FID. Perthes’ disease versus sickle cell disease hip. BMJ Rapid Response www.bmj.com/content/349/bmj.g5584/rr or http://bit.ly/1tGmuYm (18 Oct ) to Perthes’ disease by Peter Kannu & Andrew Howard, Brit Med Journal Oct 4 2014 Vol 349 pages 32-33.
384 Konotey-Ahulu FID. Ebola and Ethics: “Are vaccine trials going on somewhere in Africa?”. http://www.bmj.com/content/350/bmj.h2105/rr-5 BMJ Rapid Response 02 June 20
385 Konotey-Ahulu FID. Ebola and Ethics: Ghana Academy of Arts and Sciences and Ghana Government Suspend Ebola Virus Vaccine Trials. BMJ Rapid Response 14 June 2015 http://www.bmj.com/content/350/bmj.h2105/rr-7
386 Konotey-Ahulu FID. Ebola viewed through HIV/AIDS spectacles – What Africans think. BMJ Rapid Response. August 7 2015 www.bmj.com/351/bmj.h4142/rr-0 to Zosia Kmietowicz: Ebola vaccine trial results “extremely promising” says WHO. BMJ 351: h4192 July 31, 2015.
387 Konotey-Ahulu FID. Scientists call for moratorium on clinical use of human germline editing: A déjà vu of Ethical Caveat! www.bmj.com/content/351/bmj.h6603/rr-0 Rapid Response 16 Dec 2015 to Dr Michael McCarthy’s “Scientists call for moratorium on clinical use of human germline editing”. BMJ 2015; 351:h6603 http://www.bmj.com/content/351/bmj.h6603/rr-0
388 Konotey-Ahulu FID. Hip pain and radiographic signs of osteoarthritis: Sickle cell & other haemoglobinopathy differential diagnosis. British Medical Journal Rapid Response 8 January 2016 http://www.bmj.com/content/351/bmj.h5983/rr-2 to MJ Nieuwenjse and Rob G Nelissen BMJ 2015; 351 doI: http://dx.doI.org/10.1136/bmj.h5983 http://www.bmj.com/content/351/bmj.h5983/rr-2 (Published 2 December 2015)
391 Konotey-Ahulu FID. Will Home Office VISA Refusal Prompt West African Relatives To Vote Brexit? http://www.bmj.com/content/353/bmj.i3027/rapid-responses Rapid Response 10 June 2016
392 Konotey-Ahulu FID. Home Office VISA Refusal Prompt West African Relatives to Vote Brexit? Full Apology Now Received from Home Office. Rapid Responses June 22 2016 http://www.bmj.com/content/353/bmj.i3027/rapid-responses
393 Konotey-Ahulu FID. BREXIT: DEMOCRACY IS COUNTING HEADS REGARDLESS OF WHAT THE HEADS CONTAIN. http://www.bmj.com/content/353/bmj.i3551/rr-6 Rapid Responses June 30 2016
399 Konotey-Ahulu FID. The God Delusion title devalues sensible discourse. BMJ Rapid Response 19 October 2016.http://www.bmj.com/content/335/7629/1099.1/rr-0
401 Konotey-Ahulu FID International Medical Graduates and quality of care: What if quality of care in developing country is better than UK’s? BMJ Rapid Response March 1 in response to “International medical graduates and quality of care” by Aneez Esmail, Julian Simpson. 356:doi10.1136/bmj.j574 http://www.bmj.com/content/356/bmj.j574/rr-0
403 Konotey-Ahulu FID. Should we abandon routine blood tests? No, not when hereditary erythrocytopathy poses a real problem in a so-called multiracial population! BMJ Rapid Response to Alastair Faulkner et al and K. Siau on “Should we abandon routine blood tests?” No, do Abnormal Haemoglobin and G6PD tests routinely http://www.bmj.com/content/357/bmj.j2091/rr-15
404 Konotey-Ahulu FID. BMA AGM 2017 on Abortion – A damning verdict on my genetic defect and family members’ BMJ Rapid Response 30 June 2017 to Abi Rimmer and Rebecca Coombes on “BMA annual meeting: Doctors who carry out abortions should not face criminal sanctions, says BMA” 28 June 2017 BMJ 2017; 357: j1136 https://doi.org/10.1136/bmj.j3116 | www.bmj.com/content/357/bmj.j3116/rr June 28
406 Konotey-Ahulu FID. MEDICINES AND HARMS: Could international Fraud Unearthed In Ghana Be Happening Elsewhere? BMJ Rapid Resp 20 June 2017
www.bmj.com/content/357/bmj.j3129/rapid-responses
408 Konotey-Ahulu FID. Genetic Testing and Counselling Towards Genetic Public Health. BMJ 2017;358:j4101 Dec 21 http:www.bmj.com/content/358/bmj.j4101/rr-0
Rapid Response to Allison Streetly 28 Sept 2017 A common definition on genetic testing – can we agree on one? Re: PRACTICE article by C Semsarian & J Ingles 21 September 2017 .http:www.bmj.com/content/358/bmj.j4101/rr-0
409 Konotey-Ahulu FID. Personal Answer to The Question “Do you believe in God?” [48 References] BMJ Rapid Response to Savros Saripanidis “Do you believe in God?” Re: Kevin Barraclough “Do you believe in God? BMJ 319; doi.10.1136/bmj.7214.929a http://www.bmj.com/content/319/7214/929.2/rr-0
http://www.bmj.com/content/359/bmj.j4669/rapid
410 Konotey-Ahulu FID. There but for the grace of God …– Fiona Godlee’s Sanctified Common Sense [FGSCS] Rapid Response to There but for the grace of God F Godlee BMJ 2018; 360:k485 http://www.bmj.com/content/360/bmj.k485/rr
411 Konotey-Ahulu FID. “So You Know Where I am coming from (SYKWIACF”) Prefaces My Religious Belief Competing Interest. June 1 2018 BMJ Rapid Response https://www.bmj.com/content/361/bmj.k1558/rr-4
418 Konotey-Ahulu FID. Aviation Safety: Ghanaians recall media disinformation deriving from scientific misinformation, BMJ Rapid Resp. https://www.bmj.com/content/364/bmj.l735/rr-7 Mar 1 2019 to Partha Kar: Applying aviation safety to healthcare; are we missing the fundamental? Partha Kar 364:doi10.1136/bmj.l735
421 Konotey-Ahulu FID. Avascular Hip Necrosis: Sickle Haemoglobinopathy predominates worldwide. BMJ Rapid Response to Lamb JN et al 1 June 2019 Avascular necrosis of the hip BMJ 1 June Vol 365, p 325 (BMJ 2019; 365:l2178) https://www.bmj.com/content/365/bmj.l2178/
423 Konotey-Ahulu FID. EVIDENCE – Do not forget the hidden human dimension. BMJ 07 August 2019 Re: Holger Schunermann et al Distinguishing opinion from evidence in guidelines. BMJ 2019;366:L4606 July 19 2019 BMJ 2019; 366 doi: https://doi.org/10.1136/bmj.l4606 https://www.bmj.com/content/366/bmj.l4606/rr-11 |
424 Konotey-Ahulu FID. How-When-Where Does Common Sense Scream “The Transgenderism Emperor Has No Clothes”? British Medical Journal 18 October 2019 Re: Deborah Cohen and Hannah Barnes. Gender dysphoria in children: puberty blockers study draws further criticism. BMJ 2019; 366:l5647 https://doi.org/10.1136/bmj.l5647https://www.bmj.com/content/366/bmj.l5647/rr-5
424a Cohen Deborah, Barnes Hannah. Gender Dysphoria in children puberty blockers study draws further criticism. BMJ 2019; 366: L5647 https://doi.org/10.1136/bmj.l5647
427 Konotey-Ahulu FID. COVID-19: Treatment with CLOROQUINE or Intravenous Vitamin C Requires Prior Exclusion of G6PD Deficiency! April 8 2020. Re: Ferner Robin E, Aronson Jeffrey K. Chloroquine and Hydroxychloroquine in Covid-19. https://doi.org/10.1136/bmj.m1432 .https://www.bmj.com/content/369/bmj.m1432/rr-21 BMJ 2020; 369.m1432 April 8 2020.
428 Ayettey AS, Quakyi Isabella, Ayettey-Annie Hannah NG, Sagoe Kwamena W, Ayettey-Adamafio Mary NB, Newman-Nartey Merley, Ayettey Brew Ruth NA, Nartey Nii-Out, Amoah Albert GB, Konotey-Ahulu FID. COVID-19: A Case for Hydrogen Peroxide Mouthwash and Gargle to limit SARS-CoV-2 Infection. BMJ July 2 2020 BMJ 2020; 368: m1252 : Re: What Treatments are being investigated? Elisabeth Mahase https://www.bmj.com/content/368/bmj.m1252/rr-27 BMJ 2020; 368.m1252 March 26, 2020.
429 Konotey-Ahulu FID. COVID-19: “Few can doubt we need a covid-19 vaccine as soon as possible ..” Really? 22 August Re: Fiona Godlee, EDITORIAL. 22-29 August Vol. 370. Less haste, more safety. BMJ 2020; 370.3258 Konotey-Ahulu FID https://www.bmj.com/content/370/bmj.m3258/rr-2
432 Konotey-Ahulu FID..COVID-19: “WHAT WE EAT MATTERS ALL THE MORE NOW” SHOULD ANTICIPATE OTHER NON-VACCINE ADVICE. Re: Fiona Godlee. EDITORIAL. What we eat matters all the more now. BMJ 2020; bmj.m370 December 1, 2020. https://www.bmj.com/contact/370/bmj.m2840/rr-5 .