Responding to
Antenatal haemoglobinopathy screening
by Judy Shakespeare
BMJ 341:doi:10.1136/bmj.c5243 (Published 18 October 2010) www.bbj.com
Rapid Response http://www.bmj.com/content/341/bmj.c5243/reply#bmj_el_243447
October 25 2010 by
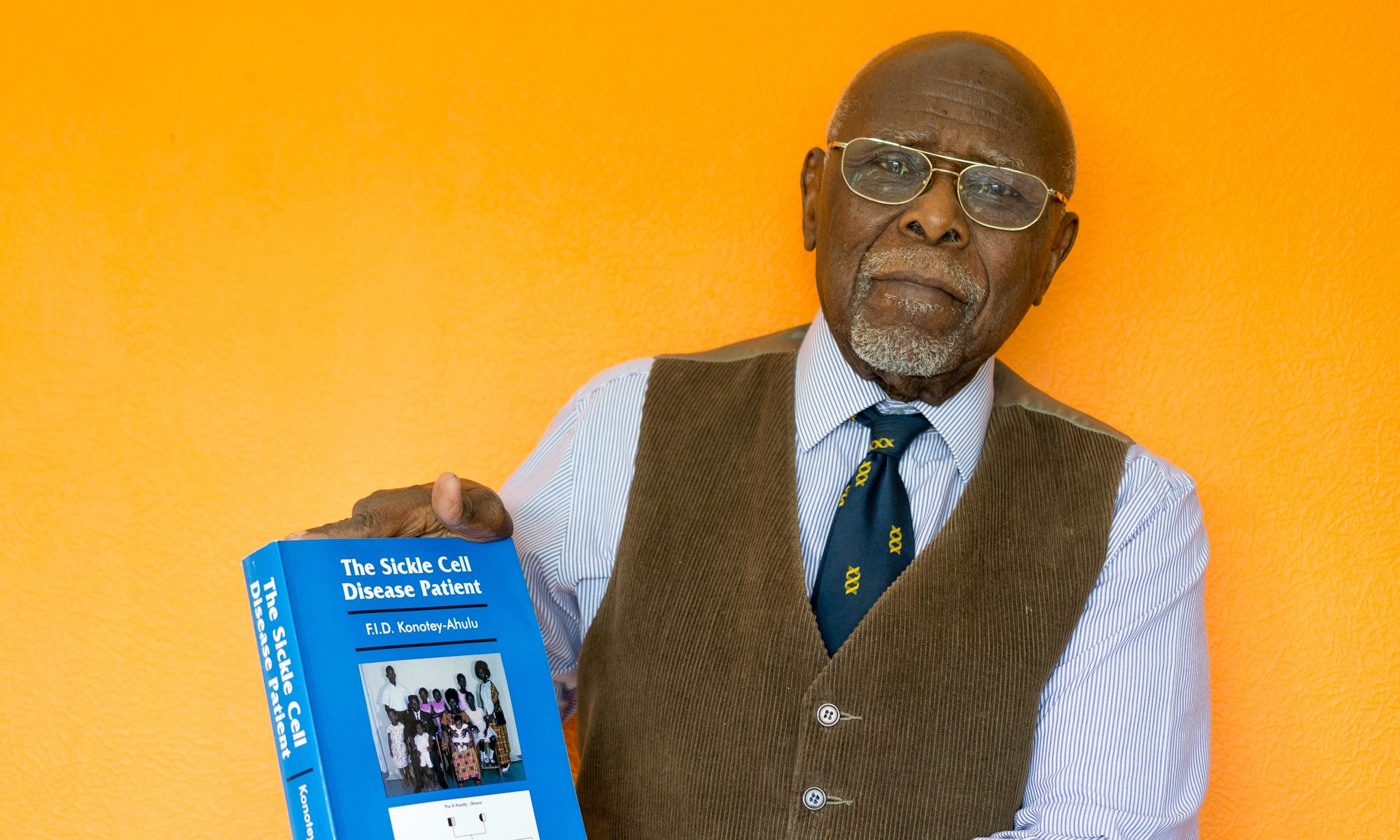
Felix ID Konotey-Ahulu, Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast , Ghana and Consultant Physician Genetic Counsellor in Sickle&Other Haemoglobinopathies 10 Harley St London W1G
The commissioned editorial [Reference 1] of Judy Shakespeare (18 October) is as comprehensive as the article [2] of Elizabeth Dormandy et al whose concerns the editorial underlined. My comments with references [3] on the Elizabeth Dormandy paper are therefore equally applicable to both articles, and will not largely be repeated here. But there are a couple of clarifications which readers would like to see made.
CLARIFICATIONS NEEDED
What does the following mean? “Antenatal screening for sickle cell disease and thalassaemia is just the tip of a genetic iceberg and primary care needs to be prepared.” [1]. How can screening be the tip of an iceberg?
Nor is the following easily comprehensible: “In the United Kingdom , about 250,000 people are healthy carriers of sickle cell gene variants and 12,500 have the disease ..”
What are healthy carriers of sickle cell gene variants? Does the author mean beta-globin gene variants? If as Judy Anderson states, her fellow general practitioners need to “raise their awareness and skills” to educate their patients are they likely to understand what “sickle cell gene variant carrier” means?
GHANAIAN BASIC TERMINOLOGY ACCEPTABLE TO EVEN ILLITERATES
Will UK General Practitioners countenance the terminology I use to instruct Ghanaian illiterates and fellow health staff with the message of sickle cell disease inheritance? For decades I have told them that all Ghanaians are divided into 3 broad phenotypes, using my own parents and their children [Reference 4] as examples: (i) ACHEACHE (those who have inherited an ACHE gene from both parents and therefore ache in the cold rainy season with sickle cell disease, like 3 of my parents’ 11 children) (ii) NORMNORM (no cold season rheumatism, like 4 of my parents’ children, having inherited no abnormal haemobglobin, and blood test shows no beta globin variant) (iii) NORMACHE (no cold season rheumatism, like the other healthy 4 of us but blood test shows one beta globin variant trait, like our parents). Every new patient of mine for several decades now has had Haemoglobin Electrophoresis done, confirming that 1 in 3 of West Africans is NORMACHE ie a Trait. In my experience, the assumption that identified NORMACHE x NORMACHE marriages will be queuing up to have prenatal diagnosis and selective abortion done when offered it is too presumptuous for the reasons already given in my earlier comments [Reference 3]. Many prefer genetic gambling, then stopping procreation after 1 or 2 children if they happen to avoid ACHEACHE phenotype. If a sickle cell disease offspring arrives, they do not panic because they know many adult ACHEACHE Achievers. [3]
SICKLE CELL DISEASE HAEMOGLOBINOPATHY IS DIFFERENT
Sickle cell anaemia, a qualitative molecular pathology ‘SS phenotype’, and beta thalassaemia major a quantitative molecular pathology are both, as Judy Shakespeare correctly points out [1] homozygous recessive, but their public health handling must be entirely different [Reference 3]. No where in the world is beta-thalassaemia minor, the heterozygote, 33.3% of the healthy population, whereas if one phenotypes West Africans anywhere in the world well above 35% of us will be NORMACHE, ie traits of abnormal haemoglobins (AC or AS), and we do not know it until we are investigated by Hb electrophoresis. Helping Ghanaians and Nigerians to make informed decisions in procreation does not lie in prenatal diagnosis and selective abortion as appears to be the case in Cyprus , but does lie in Genetic Counselling with Voluntary Family Size Limitation. [References 4 & 5]. And, take it from me, that works!
Felix I D Konotey-Ahulu MD(Lond) FRCP DTMH ORDER OF THE VOLTA ( GHANA )
Dr Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast , Ghana and Consultant Physician Genetic Counsellor in Sickle and Other Haemoglobinopathies. [felix@konotey-ahulu.com]
Conflict of interest: My parents who were traits for abnormal haemoglobins, had 11children 3 of whom had sickle cell disease, 4 are traits and 4 have no beta globin gene variant.
1 Shakespeare Judy. Antenatal haemoglobinopathy screening. BMJ 2010; 341: c5243 (Editorial 18 October)
2 Dormandy Elizabeth, Gulliford Martin, Bryan Stirling, Roberts Tracy E, Calnan Michael, Atkin Karl, Karnon Jonathan, Logan Jane, Kavalier Fred, Harris Hilary J, Johnston TraceyA, Anionwu Elizabeth N, Tsianakas Vicki, Jones Patricia, Marteau Theresa M. Effectiveness of earlier antenatal screening for sickle cell disease and thalassaemia in primary care: cluster randomised trial. BMJ 341:doi:10.1136/bmj.c5132 (5 October 2010)
3 Konotey-Ahulu FID. Antenatal screening for sickle cell disease and beta-thalassaemia. http://www.bmj.com/content/341/bmj.c5132/reply#bmj_el_242914 BMJ Rapid response. 12 October 2010
4 Konotey-Ahulu FID. Sickle cell disease in successive Ghanaian generations for 3 Centuries. http://www.konotey-ahulu.com/images/generation.jpg
In The Human Genome Diversity Project: Cogitations of An African Native. Politics and the Life Sciences (PLS) 1999, Vol 18: No 2, pp 317-322. [Invited Commentary on Professor David Resnik’s article: The Human Genome Diversity Project: Ethical Problems and Solutions] PMID: 12561789 [PubMed – indexed for MEDLINE]
5 Konotey-Ahulu FID. Sickle Cell Disease: The Case for Family Planning. Accra . ASTAB Books, Ltd 1973
Competing interests: My parents who were traits for abnormal haemoglobins, had 11 children 3 of whom had sickle cell disease, 4 are traits and 4 have no beta globin gene variant.