Blaming sudden death on Sickle Cell Trait?
Flaws In Article Of Charis Kepron, Gino Somers and Michael Pollanen Exposed.
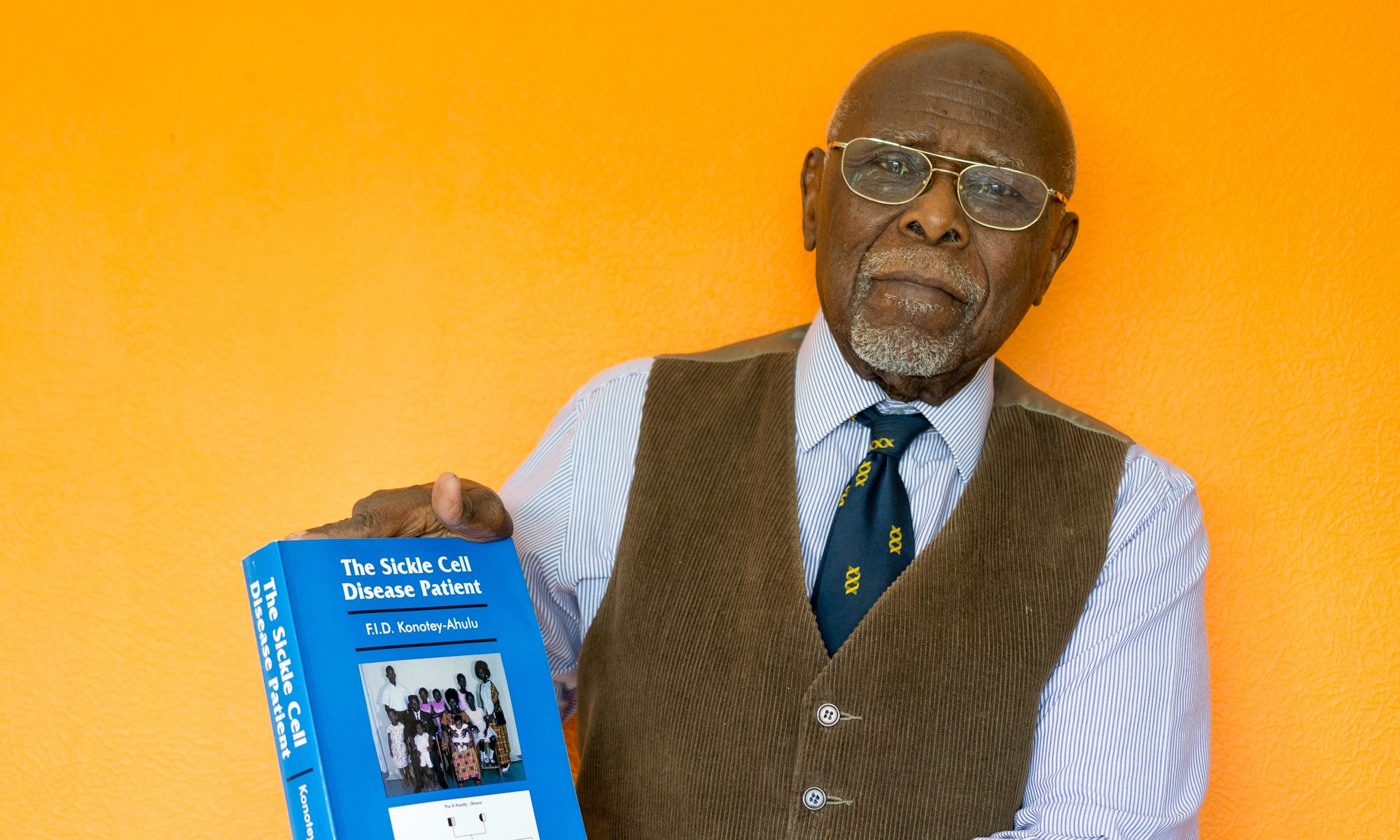
Felix I D Konotey-Ahulu MD(Lond) FRCP(Lond) DTMH(L’pool) FGCP FWACP FTWAS
Dr Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast, Ghana and Consultant Physician Genetic Counsellor in Sickle Cell and Other Haemoglobinopathies, Ten Harley Street, London W1G 9PF. [Founder & Co-Director of KÁGÈ SICKLE CELL FOUNDATION www.sicklecell.md & felix@konotey-ahulu.com]
“Sickle Cell Trait Mimicking Multiple Inflicted Injuries in a 5-Year-Old Boy” is the title of an article published in the Journal of Forensic Science 1. I do not know which expert reviewed and passed this article for publication but the 20% of healthy Ghanaians with sickle cell trait have good reason to protest at such a flawed article masquerading (as the authors Charis Kepron and others put it) “the first to describe sickle cell trait pathology as a mimic of a non-accidental injury”1.
The defects of this article are very many:
(i) Mentioning sickle cell disease (scd) and sickle cell trait (sct) in the same breath betrays clinical ignorance. References 1 and 2 on “sickle cell disease” quoted by Kepron and colleagues in support of a “sickle cell trait” article are therefore totally irrelevant.
(ii) Ponder the following statement of the authors: “Sudden unexpected death in a 5-year old child due to pulmonary complications of sickle cell trait in whom the pattern of bone lesions seen at autopsy mimicked multiple inflicted injuries”.1 Now, 1 in 5 of all Ghanaian children at home and abroad who may be found to be traumatised and left with broken bones will be found to be sickle cell trait because 20% of the rest of the healthy Ghanaian population are also sickle cell trait ‘AS’. So does that mean the bone defects seen in this Ghanaian child in Canada can be attributed to sickle cell trait?
(iii) The child had complained of a painful leg, and was said to have had “mild tissue swelling” and yet the X-ray films were not “retrospectively reviewed”.1 Why?
(iv) There was no family study of sickling in a case report of such importance. What were the levels of Haemoglobin ‘S’ in the mother and/or the father?
(v) The haemoglobin electrophoretic report is flawed. Add up the various fractions quoted in the publication and you get 100% [Hb A = 74.9%, Hb S = 23.2%, Hb F = 1.9%], but where is Haemoglobin A2? How could reputable haematologists, paediatricians, and pathologists forget Hb A2 in such an electrophoretic report?
(vi) Autopsy showed the Right lower lobe of the lung to be (in their own words) “pale, congested, consolidated, and focally haemorrhagic”. The question is this: Are these pneumonic changes never seen in children who do not have sickle cell trait? In other words, does sickle cell trait have to be invoked to explain such pathological changes?
(vii) “A layered dissection of the posterior para-spinal muscles of the neck” say the authors “showed focal areas of soft tissue haemorrhage”1 and yet they blame these changes on sickle cell trait, ruling out child abuse?
(viii) The authors Charis Kepron, Gino Somers and Michael Pollanen report that “Both lungs contained foreign material in keeping with aspiration of gastric contents”, the classical residue for an aspiration pneumonia that could kill a child instantly, yet the sudden death was attributed to sickle cell trait by these authors?
(ix) Staphylococcus aureus was cultured from both lungs, and yet complicated staphylococcal pneumonia was not suggested as the cause of sudden death, but the sickle cell trait with just 23.2% of sickle cell haemoglobin ‘S’ ?
(x) The authors state that the sickle cell trait “can be a cause of acute complications normally associated with sickle cell disease including the acute chest syndrome”.1 This ex cathedra statement is simply not true. The sickle cell trait ‘AS’ had run at Olympic Games at Mexico City over 7000 ft where the air is thin and oxygen concentration is lower than at sea level, and these sickle cell traits ‘AS’ (or NORMACHE as I call them) had competed with and beaten the whole world. And the authors couple this ‘AS’ phenotype with Sickle Cell Disease phenotype (ACHEACHE)? Moreover, people of all nationalities without sickle cell trait die suddenly from aspiration pneumonia, so why should a sickle cell trait child behave differently?
(xi) Invoking acute chest syndrome as cause of death in a sickle cell trait child stems more from ignorance of what has been termed “acute chest syndrome”. The term was coined only in recent decades to explain breathing problems in sickle cell disease patients. This diagnosis assumed huge proportions only when Morphine and Diamorphine constituted the recommended prescription to treat pain of sickle cell crisis in the UK and the USA2. The NCEPOD Report of the United Kingdom revealed that “Nine out of the 19 patients with sickle cell disease who had pain on admission and who then died had been given excessive doses of opiods” (meaning morphine and diamorphine)“ 3, 4, 5. Now, for Kepron and colleagues to invoke the acute chest syndrome as contributory to the Ghanaian child’s sudden death in Canada was just scraping the barrel to link sickle cell trait to the sudden death. Quoting Vichinsky and colleagues 6 in support of their acute chest syndrome proposition was a mistake because Vichinsky’s paper failed to diagnose the devastating role of opiates (Morphine and Diamorphine) in the causation of the chest syndrome due to the opiods’ respiratory depressive effect on the very patients who needed oxygen to survive. 5
(xii) The authors’ references 11 and 12 in the article that they cite to blame acute chest syndrome on sickle cell trait failed to take cognisance of the ten Addae’s Critreria 7 which must be met before serious symptomatology is blamed solely on sickle cell trait. For instance, the sickle cell trait must not be blamed for serious symptomatology without quantification of Hb A2 and yet Kepron and colleagues did not even mention Haemoglobin A2 let alone quantify it.
(xiii) It is quite surprising how facts that should have made Kepron and colleagues look elsewhere, rather made them fixate on sickle cell trait because they were determined to do just that. Take for example their statement “Although the clinical information required for a diagnosis of acute chest syndrome was missing …” histologic findings were used by them to “prove” acute chest syndrome, and they stated that “acute chest syndrome was felt to be the major contributing factor to the cause of death”.1 Does the phrase “was felt” have any place in scientific discussion? Should we be concerned with how we “feel” when debating scientific topics, or should we rely on facts alone?
(xiv) The final statement of their inauspicious article says it all; it betrays a deliberate desire to link the un-linkable: “Although Sickle Cell Disease/Sickle Cell Trait is not one of the classic mimickers of child abuse, unusual orthopaedic pathologies can and do occur, and may appear as inflicted injury on skeletal survey”1.
(xv) The authors Kepron, Somers, and Pollanen fail to do their home work in the country that discovered Haemoglobin Quebec-Chori. This haemoglobin masquerades as normal adult Haemoglobin ‘A’ but which when tagged on to sickle cell haemoglobin does not produce sickle cell trait ‘AS’ (ie NORMACHE by my terminology), but rather sickle cell disease (ACHEACHE). This was how I put it in The Lancet in a communication entitled ‘Beware of symptomatic sickle-cell traits’: 8
“With the sickle cell population increasing yearly in the UK, the finding by Witkowska and colleagues9 of sickle cell Haemoglobin Quebec-Chori genotype producing a sickle cell disease phenotype masquerading electrophoretically as a sickle cell trait makes it vital for clinicians to probe further any case of sickle cell trait where the symptoms suggest sickle cell disease.9 Many individuals with true sickle cell trait ‘AS’ (betaA3[6Glu; betaA3[6Glu à Val]) with ‘A’ greater than ‘S’ have been victimised in respect to employment and life insurance because of substandard medical reports in journals”. 10, 11
The authors of this present article do not appear to have read about Haemoglobin Quebec-Chori which was first discovered in their own country Canada.9
LESSONS DRAWN FROM THIS ‘JOURNAL OF FORENSIC SCIENCE‘ ARTICLE
1. Battles that have been fought and won in the Sickle Cell Trait controversy can suddenly be resurrected, so there is need to be vigilant. Forty years ago, based on a false report by authors who had never been to Ghana, on a Ghanaian sickle cell trait during the 45-minute flight from Kumasi to Accra it was suggested that for their own safety “Negro passengers” should be tested at airports for the sickling phenomenon “for their own safety”12 Ghanaian experts exposed not only the falsehood of the report13, but also were instrumental in reversing draconian measures that were being taken world wide based on that false report. Black pilots and air crew had been grounded at Kennedy Airport in the USA because of the false report. It was Ghanaian expertise that restored them to flying duties, and forced the case report publication in the British Medical Journal to be withdrawn.14 [See the detailed account in FAQs – Frequently Asked Questions on my website www.konotey-ahulu.com or www.sicklecell.md] 15
2. University of Illinois Professor of Medicine and Pathology Dr James Boweman MD and Dr S. Bernstein observing the spate of journal articles linking all kinds of symptoms with the sickle cell trait were forced to exclaim when a Black man beaten to death in police custody was found to be sickle cell trait, and the death was then attributed to the sickle trait: “Persons with sickle cell trait will no longer be able to become ill or even die lest they find themselves subject of a case report”.10 This prediction of Boweman and Bernstein in 1977 regarding bogus articles has sadly been fulfilled through this flawed case report of Charis Kepron and colleagues.1
3. New attempts are being made presently (in this year of 2011) to ban sickle cell traits from competing in athletics because sudden death has been linked (spuriously) to the sickle cell trait phenotype as recounted in my book.11 My website FAQs have dealt with the flawed articles cited in this respect. If someone who does not sickle dies from exercise, that is considered natural, but when sickle cell trait is found in the person, then it is not considered “natural” – it must be due to the sickle cell trait. Banning 20 per cent of all Ghanaian international athletes (and Black competitors in general) from global athletics “for their own safety” is seriously being considered by some scientists of World Bodies. Some of them talk about “Black Sickle Cell Traits” forgetting that 1 in 6 of the White people in southern Turkey 16, 17 and up to 30% of the white people in Greece around where Lake Kopais was had been shown to have the sickle cell trait (‘AS’) 18, 19 leading Ghana’s Dr Frank Djabanor once to ask in the British Medical Journal: “How can we identify them by their external features to thrust upon them the benefits of this advice”? 20, namely the advice that Negro passengers should be tested at airports for sickle cell trait “for their own safety” 12 The term “Black Sickle Cell Traits” must be banned, because there are millions and millions of “White Sickle Cell Traits”. Insurance Companies, and International Sports Federations need to take note of that. If they do not, they must be held to account. Indeed I once pointed out 21 that when contacted in the USA by Professor James Boweman “about the harmless sickle cell trait”, 41% of 39 insurance companies admitted to loading the trait premium. “It is my understanding” added Boweman “that insurance companies generally test only Blacks for the sickle cell trait”.22
4. What I have said above is no joking matter. African doctors should be aware of global trends that are inimical to their welfare. Articles like that of Kepron et al encourage Insurance Companies to load the premium of Sickle Cell Traits because of the unjustified and unscientific published statements like “Complications of Sickle Cell Disease/Sickle Cell Trait are not usually on the differential diagnosis of traumatic injury”.1
5 Articles such as we find here in the Journal of Forensic Science are likely to be quoted by inexperienced clinicians and pathologists in support of their equally flawed findings. This must not be allowed to happen. Fortunately, wise editors such as are found for The British Medical Journal and The Lancet in England always go back to correct errors in previous publications whenever these were later pointed out to them. “We therefore wish to withdraw this case”14 was how Green, Huntsman and Serjeant removed the unsubstantiated “sickle cell trait intestinal infarction” case from publication. Family studies have shown that a case I once thought was sickle cell trait (NORMACHE), was in fact the Ghanaian sickle cell haemoglobin C disease patient (ACHEACHE) who was a banker and who died under anaesthesia in a London hospital during eye surgery. I challenge the editors of Journal of Forensic Science, in the light of what has been said above, to state that the case for child abuse in their case report of the second autism child that they described could not be dismissed, and I urge that these authors’ conclusion that their findings could be attributed to sickle cell trait be dismissed forthwith.
6 There are huge financial interests involved if the true sickle cell trait ‘AS’ (NORMACHE) who beat the whole world at athletics is equated with sickle cell disease pathology, allowing insurance companies to benefit at the expense of healthy people. As Cambridge University’s Professor Hermann Lehmann, the doyen of Abnormal Haemoglobin research in the UK, wrote to the London Times when the false sickle cell trait story was published on December 9 1971 advocating the removal of sickle cell traits from flying duties: “The sickle cell trait is, in some Africans much more rare than in the population of, say Crete or Coimbatore” and he went on to say that “sickle cell carriers competed without ill effect at the Olympic Games at Mexico at an altitude of 7000 ft”23 Fancy then a Black athlete coming down from Mexico City to New York at sea level and be told that his Health Insurance premium would go up to 150% because some researcher had published that exercising at 4000 ft had caused death in a sickle cell trait! For the world to be told at the Martin Luther King Jr Foundation Award Ceremony in 1972 in Philadelphia in the presence of Abnormal Haemoglobin Nobel Prize winners Linus Pauling and Max Perutz, that Insurance Companies in the USA were benefiting unfairly from the “Sickle Cell Trait sudden death at 4000 ft” story – a story that lacked scientific veracity – for the world to be told this – was too much of a risk to take so the organisers of the Award Ceremony provided me whom they had invited to give the Keynote Address on “The difference between Sickle Cell Trait and Sickle Cell Disease” with four body guards for all the time I was in Philadelphia. Read the full story in the British Medical Journal.24
7 Finally, please wake up to the fact that modern researchers fail to recognise and quote thorough work that had been done decades ago. Any modern author that relies on a MEDSEARCH that contents itself with going back only 25 years is deceiving not only themselves but also the rest of us. Professors George M Edington and Hermann Lehmann did such meticulous Abnormal Haemoglobin research in the Gold Coast (Ghana) nearly 60 years ago as has hardly been equalled in thoroughness. 25-29 What these giants of Abnormal Haemoglobin Research said about Sickle Cell Trait and Sickle Cell Disease all those decades ago has not been bettered by any subsequent work that I know of. Yet modern authors like Kepron and colleagues not only do not refer to them, but rather claim to have discovered new insights into how sickle cell traits present. Professor Bela Ringelhann and I have summarized (with no less than 225 references) much of this and subsequent work.30 Ignoring this material because much of it was published decades ago is doing a great deal of disservice not only to Medical Science but also to us West Africans 1 in 3 of whom is carrying a beta-globin gene variant (NORMACHE).
References
1 Kepron Charis, Somers Gino R, Pollamen Michael S. Sickle Cell Trait Mimicking Multiple Inflicted Injuries in a 5-Year-Old Boy. Journal of Forensic Science Volume 54, No.5, pp 1141 t0 1145 September 2009.
2 Konotey-Ahulu FID. Morphine for painful crisis in sickle cell disease. Brit Med J 1991; 302: 1604
3 Mayor Susan. Enquiry shows poor care of patients with sickle cell disease. Brit Med J 2008; 336: 1152
4 NCEPOD (National Confidential Enquiry into Patient Outcome and Death) .. produced an 84-page report entitled ‘SICKLE: A Sickle Crisis? (2008)’ The Report (www.ncepod.org) ‘reviews the circumstances around deaths of in-patients with Haemoglobinopathies – sickle and beta-thalassaemia in the 21st Century in England, Wales, Northern Ireland, and the off-shore islands’…’Nine out of the 19 patients with sickle cell disease who had pain on admission and who then died had been given excessive doses of opiods’’. Death that was put down to “Acute Chest Syndrome” clearly was due to respiratory depression from the drugs which further produced in vivo sickling.
5 Konotey-Ahulu FID. Poor care for sickle cell disease patients: This wake up call is overdue BMJ Rapid Response May 28 2008 BMJ 2008; 336: 1152 http://www.bmj.com/cgi/eletters/336/7654/1152a#196224 to Susan Mayor “Enquiry shows poor care for patients with sickle cell disease” on National Confidential Enquiry into Patient Outcome and Death (NCEPOD) REPORT “SICKLE: A Sickle Crisis? (2008) info@ncepod.org
6 Vichinsky EP, Neumayr LD, Earles AN, Williams R, Lennette ET, Dean D, et al. Causes and outcomes of the acute chest syndrome in sickle cell disease. National Acute Chest Syndrome Study Group. New England J Medicine 2000; 342(25): 1855-66.
7 Addae RO. Sickle cell trait and altitude. Br. Med J 1972; 1: 53.
8 Konotey-Ahulu FID. Beware of symptomatic sickle cell traits. Lancet 1992; February 29, p 555.
9 Witkowska HE, Lubin BH, Beuzard Y et al. Sickle cell disease in a patient with sickle cell trait and compound heterozygosity for haemoglobin S and haemoglobin Quebec-Chori. New England Journal of Medicine 1991; 325: 1150-1154. [Note that the title of this article is incorrect: Sickle cell trait cannot also be referred to as sickle cell haemoglobin Quebec Chori disease. The ‘AS’ pattern is sickle cell trait pattern, but the ‘A’ here is not a true ‘A’ but the new haemoglobin called Quebec-Chori, producing a disease phenotype, not a trait phenotype].
10 Boweman JE, Bernstein S. Caution about preliminary reports. Pediatrics 1977; 59: 639-640.
11 Konotey-Ahulu FID. “Percentage values of haemoglobins S, F, A2, C, A in various sickle cell phenotypes, and consideration of the Sickle Cell Trait”, In The Sickle Cell Disease Patient: Natural History from a Clinico-epidemiological study of the First 1550 patients of Korle Bu Hospital Sickle Cell Clinic. Macmillan London 1992 & T-A’D Co Watford 1996, Chapter 30, pages 349 to 371.
12 Green RL, Huntsman RG, Serjeant GR. Sickle cell and altitude. Br Med J 1971; 4: 593-595.
13 Konotey-Ahulu FID. An International Sickle Cell Crisis. Ghana Medical Journal 1972; 11: 4-8.
14 Green RL, Huntsman RG, Serjeant GR. Brit Med J 1972; 2: 294
15 Konotey-Ahulu FID. Frequently Asked Questions (FAQs) in www.sicklecell.md or www.konotey-ahulu.com 2001 – 2011.
16 Aksoy M. Sickle cell trait in Southern Turkey. Lancet 1955; 1: 589-590.
17 Altay C, et al. Haemoglobin S and some other hemoglobinopathies in Eti-Turks. Human Heredity 1978; 28: 56-61.
18 Choremis C et al. Sickle cell anemia in Greece. Lancet 1951; 1: 1147
19 Choremis C et al Blood groups of a Greek community with a high sickling frequency. Lancet 1957; 2: 1333-34
20 Djabanor F F T. The Sickle Cell Trait and Altitude. Brit Med J 1972. 1: 113.
21 Konotey-Ahulu FID. Insurance and genetic testing. Lancet March 3 1993, page 833.
22 Boweman J E. Ethical, legal and humanistic implications of sickle cell programs. INSERM 1975, 44: 353-378.
23 Lehmann Hermann. Sickle cell and flying. The Times (London), 4th January 1972, editorial page.
24 Konotey-Ahulu FID. Four body guards and the perils of unmasking scientific truths. Brit Med J 2007; 335: 210-211, July 28.
25 Edington GM. Sickle cell anaemia in the Accra district of the Gold Coast. A review of 20 cases. Brit Med J 1953; 2: 957-961
26 Edington GM, Lehmann H. Expression of the sickle cell gene in Africa. Brit Med J 1955a; 1: 1308-11
27 Edington GM, Lehmann H. Expression of the sickle cell gene in Africa. Brit Med J 1955b; 2: 1328
28 Edington GM, Lehmann H. The sickle cell gene. Am J Clin Path 1956a; 26: 553-56
29 Edington GM, Lehmann H. Sickle cell trait in Africa. Bull WHO1956b; 15: 837-852
30 Ringelhann B, Konotey-Ahulu FID. Hemoglobinopathies and thalassemias in Mediterranean areas and in West Africa: Historical and other perspectives 1910 to 1997 – A Century Review. Atti dell’Accademia dell Science di Ferrara (Milan) 1998; 74: 267-307.
Acknowledgements: I thank Professor Simon Dyson for drawing my attention to the article of Charis Kepron and colleagues. Professor Dyson has done much to alert people to the harm that unfair publications on sickle cell states can do. I recommend his websites for study.
Simon Dyson is Professor of Applied Sociology
Room 1.27 Hawthorn Building
De Montfort University
Leicester LE1 9BH
+44 (0)116 257 7751
sdyson@dmu.ac.uk
http://www.sicklecelleducation.com
http://www.sicklecellanaemia.org
See for instance his book: Sickle Cell and Deaths in Custody
—————————————————————————————–