Dr Margaret McCartney highlights something most doctors ignore [1] Her “seams of multiple misinformation” become disinformation when deliberate, as when “Journal agrees to retract paper after university found study was never done” [2].
“EVIDENCE” AND “TRUTH” ARE WORDS NEEDING CAREFUL SCRUTINY#
“There is no real evidence that e-cigarettes do any harm”, is interpreted as “e-fags are harmless”. No evidence is increasingly used as evidence [3]. Prefix “scientific” to “truth”, and Einstein expects integrity. [4] When three doctors confessed that tests they published had been done were in fact not done I concluded letter to BMJ Editor Dr Martin Ware:
“Your readers, Sir, are interested in scientific truth. I am one of them, and the very least I am entitled to expect is that if evidence obtained from my own country cannot be scientific it should at least be true. – I am etc., F I D KONOTEY-AHULU” [5]
BUT WHAT IF TWO OR MORE EXPERTS DISAGREE ON WHAT IS TRUTH?
Lord Solly Zuckerman FRS said in his excellent article “Pride and Prejudice in Science” that disagreements about truth were often coloured by prejudice, and sometimes fraud. [6] I’ve discussed elsewhere experts’ disagreements. [7]. That Ethics is deprecated and Science re-defined by some scientists is sad. Two examples: (a) Design in nature is now not science [8]. (b) Programmes to genome-sequence whole populations anonymously [9 10] against which I have protested, indicating how dangerous this is in an “Anti-truth world” [11]. Had James Watson been genome-sequenced anonymously would the truth have come out?
NOBEL LAUREATE PROFESSOR JAMES WATSON IS AFRICAN
James Watson announced that the current global genome-sequencing exercise would show that Africans were less intelligent than other “races” [12], using the term “race” just as Charles Darwin had done: “The Origin of Species By Natural Selection – Or The Preservation Of Favoured Races In The Struggle For Life” [13]. Watson’s three to four trillion DNA bits in his genome were sequenced only to discover that his great-grandparent was African [14]. Convinced he belonged to the “favoured white race” he in fact had a great-grand parent from the African “un-favoured race”. I commented: “Watson, still alive today in the USA, was thus brutally reminded not only that there is but one human race, but also that African genes contributed to the Nobel Prize in ‘Physiology or Medicine’ which he jointly won with Francis Crick and Maurice Wilkins in 1962 on the DNA Double Helix” [15]. James Watson’s opinion was taken as scientific truth because Nobel Laureates are not supposed to be economical with the truth. The Human Genome Project became suspect [11 16 17], and this exposes the
real problem with research in Human Sciences including IQ, Linguistics and even History. Researchers wax eloquent about “Evolutionary Ethics”, making ex cathedra statements like “The capacity to develop ethics is a product of biological evolution” [18]. Such Evolutionary Fundamentalism is considered “scientific truth” while “GOD commanded, and universe materialized” [19] is ridiculed?
EVOLUTION PROFESSORS J Z. YOUNG AND PAUL R. EHRLICH
Three events in a Lecture Series on Evolution by J Z Young FRS at University College London [20] convinced me that Darwin’s Evolution by Natural Selection never took place. It was more than 3 decades later that another Fellow of the Royal Society Professor Fred Hoyle would confirm my judgement: “How has the Darwinian theory of evolution by natural selection managed, for upwards of a century, to fasten itself like a superstition on so-called enlightened opinion? Why is the story still defended so vigorously?” [21] First event (a): J Z Young was comparing the brain of a new-born human baby with that of an adult chimpanzee [20]. His words “I do not know …” stunned me and Shirley Knight sitting together. (b) One student’s question “Why …?” brought the answer: “’Why?’ questions are not permitted here” (c) J Z Young kept saying “Theory of Evolution” over and over again. This world-authority on the human brain [22] who taught me not only “what to think” to pass exams, but also “how to think” to enable me criticise my teachers, led me to the conclusion I found Professor Fred Hoyle arriving at 3 decades later, namely that Darwin’s Evolution Emperor has no clothes! But then comes Paul Ehrlich [18] sprinkling his 531-page Evolution book with “Why?” questions that he blithely proceeds to answer with ex cathedra pronouncements!
DR MARTYN LLOYD-JONES’ BOOK “TRUTH UNCHANGED UNCHANGING” [23]
This Welsh Genius [24] proved some “Truths” to be supra-scientific. [23]. I once wrote: “There is a vast area of man’s experience called the spiritual realm which neither Freudian psychoanalysis nor the scientific method can fathom” [25] Dr Lloyd-Jones’ books “Spiritual Depression” [26] and “Conversions Psychological and Spiritual” [27] support this. Because “approaches to scientific truth and spiritual truth are different” [25] one scientist will read Spiritual Depression “with much profit while another, with the same qualifications, will find it unintelligible” [25]. Dr Lloyd-Jones totally dismisses Darwin’s “races”. He recognises only intra-racial marriages: Google “Felix and Rosemary” [28].
INTERNET’S MINUS AND PLUS WITH REGARD TO TRUTH
Misinformation that Margaret McCartney mentions [1] can be counterbalanced using the same Internet when editors refuse to publish corrections [29]. Are Margaret’s two prescriptive suggestions [1] capable of identifying scientific liars [30-32] and lying journalists who suppress truth about Statins or whatever? [29]
PERSONAL QUEST FOR TRUTH
“Did that happen?” is my best question to unravel truth. Was I born on a Saturday? Was I struck by lightning on a Friday 2 days before Christmas? Science can never be used to substantiate the truth behind these events [3 33-36], so why do we defer to Science to verify infinitely more important events defining Christmas? History beats Science [37]. Dismiss me as a creationist sermonizing, and I respond: a creationist is ‘a c’; I prefer to reverse the letters and be known as ‘C a’ – “CREATOR acknowledger” whose MILLENNIUM Hymn http://bit.ly/cRrZ0s spells out supra-scientific Truth [38] about The PERSON who said “Before Abraham was I AM” [39].
Conflict of Interest: Believer in The Lord Jesus Christ [Nuntsɔ Yesu Kristo]
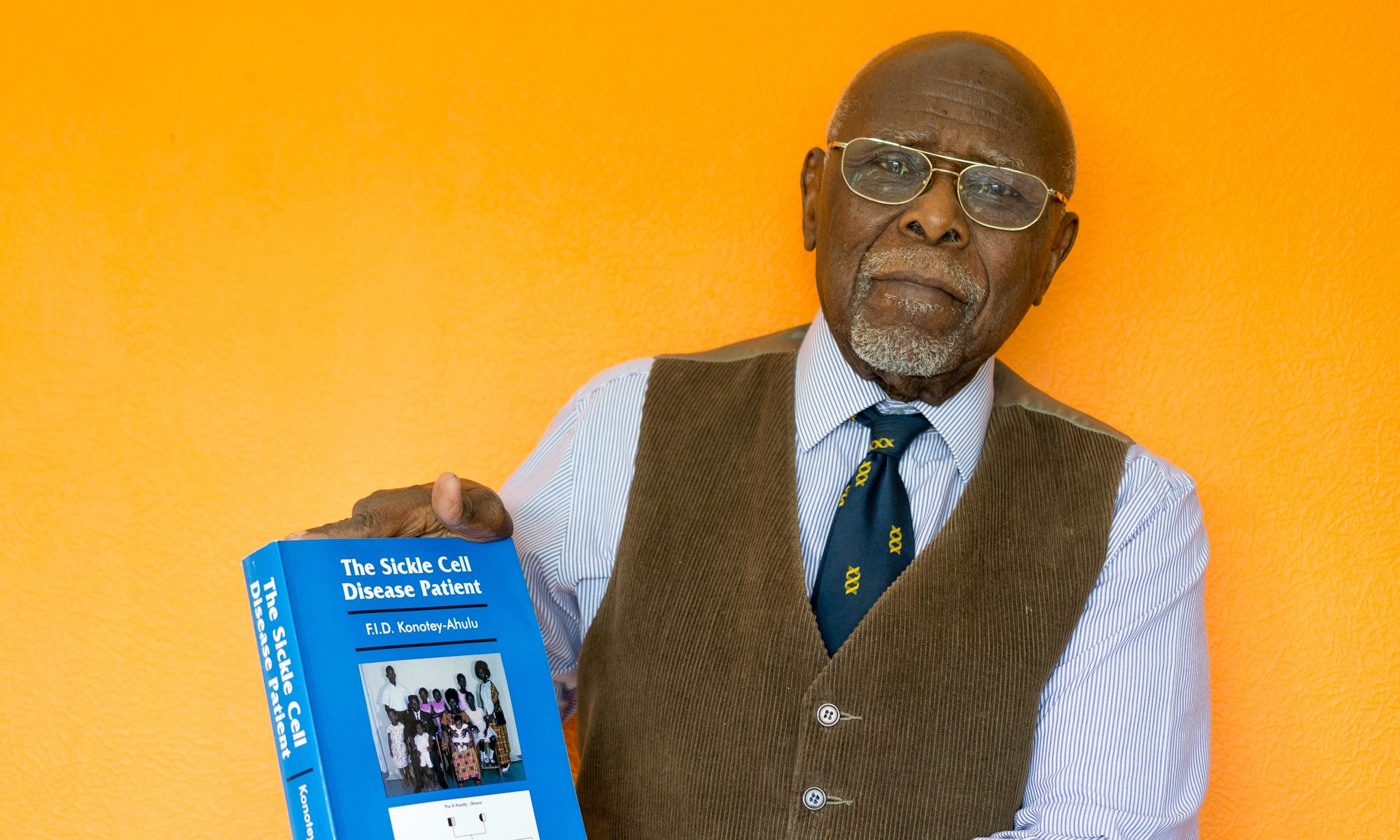
Felix I D Konotey-Ahulu FGA MD(Lond) FRCP(Lond) FRCP(Glasg) DTMH(L’pool) FGCP FWACP FTWAS Kwegyir Aggrey Distinguished Professor of Human Genetics University of Cape Coast Ghana & Former Consultant Physician Genetic Counsellor in Sickle Cell and Other Haemoglobinopathies, 9 Harley Street, London W1G 9AL.
felix@konotey-ahulu.com Twitter@profkonoteyahul
References
1 McCartney Margaret. Evidence in a post-truth world. BMJ 2016; 355: 16363 November 28, 2016
2 Dyer Clare. Journal agrees to retract paper after university found study was never done. BMJ 2013; 347: f55
3 Konotey-Ahulu FID “Private Thoughts: There is no evidence that I was born on a Saturday. Postgraduate Medical Journal of Ghana 2012; 1: 32-33 33” which often proved superiority of history over science in arriving at truth.
4 Einstein Albert “Science can be created only by those who are thoroughly imbued with the aspiration toward truth and understanding” In EINSTEIN: Life and Universe, by Walter Isaacson, New York 2007, Simon & Schuster, page 390 of 675 pages.
5 Konotey-Ahulu FID. Sickle cell and altitude. BMJ 1972; 2: 231-232.
6 Zuckerman Solly. Pride and Prejudice in Science. Aerospace Medicine 1974. 45: 638-647. (Also republished in Ghana Medical Journal 1975; 14: 52-60)
7 Konotey-Ahulu FID. Clinicians facing conflicting recommendations: Use Common sense? BMJ Rapid response Dec 5 2008 www.bmj.com/cgi/eletters/337/nov28_2/a2530#205677
8 Sarfati Jonathan. By Design – Evidence for Nature’s Intelligent Designer – The God of the Bible. Creation Book Publishers 2008 Atlanta Georgia, USA www.creationbookpublishers.com [260 pages]
9 Wise Jacqui. Consortium hopes to sequence genome of 1000 volunteers. BMJ 2008; 336: 237 (2 February)
10 Announcement: http://www.1000genomes.org/files/1000Genomes-NewsRelease.pdf International Consortium Announces the 1000 Genomes Project. Major Sequencing Effort Will Produce Most Detailed Map of Human Genetic Variation to Support Disease Studies. (Tuesday January 22 2008)
11 Konotey-Ahulu FID. 24 Konotey-Ahulu FID. Sequencing genome of 1000 volunteers: Why do this anonymously? African Journal of Health Sciences 2011; 18: 37-52 www.ajhsjournal.or.ke/admin/current/914vpjkSBOS.pdf
12 Watson James in Sunday Times: Racial differences in intelligence: James Watson, Nobel Prize winning geneticist persecuted for scientific truth. He claimed that black people were less intelligent than white people and the idea that “equal powers of reason” were shared across racial groups was a delusion. Human-Stupidity (Admin) March 14 2010. http://www.independent.co.uk/news/science/fury-at-dna-pioneers-theory-africans-are-less-intelligent-than-westerners-394898.html
13 Darwin Charles R. Origin of Species by Means of Natural Selection, or The Preservation of the Favoured Races in the Struggle for Life. John Murray, London 1859.
14 Verkalk Robert. Revealed: Scientist who sparked racism row has black genes/The Independent www.independent.co.uk > News> Science 9 December 2007
15 Konotey-Ahulu FID. There is but one human race. New African (London) December 2009, Number 490, page 4.
16 Konotey-Ahulu FID. The Human Genome Diversity Project: Cogitations of an African Native. In POLITICS AND THE LIFE SCIENCES, September 1999, Vol. 18(2), pp 317-322.
17 Konotey-Ahulu FID. Why should Africans fear any human genome project? Africawatch. November 2010, pages 34-36.
18 Ehrlich Paul R. Human Natures – Genes, Cultures, and the Human Prospect. Island Press/Shearwater Books, Washington DC 2000, page 308.
19 Holy Bible. (a) Psalm 30 verses 8 & 9: Let all the earth fear JEHOWAH. Let all the inhabitants of the world stand in awe of HIM. For HE spoke and it was done. He commanded, and it stood fast & (b) Hebrews chapter 1 verses 1 &2: God …has in these last days spoken to us by His SON, Whom HE has appointed heir of all things, through Whom also HE made the worlds & (c) Colossians chapter 1 verses 16 & 17 For by Christ all things were created that are in heaven and that are on earth, visible and invisible …all things were created through HIM and for HIM & (d) St John chapter 1 verses 1 to 3: In the beginning was the Word, and the Word was with God, and the Word was God. All things were made through Him, and without Him nothing was made that was made.
20 The God Delusion title devalues sensible discourse BMJ Rapid Response Oct 19 2016
www.bmj.com/content/335/7629/1099.1/rr-0
21.. Hoyle Fred. The Intelligent Universe. Michael Joseph, London, 1985, page 25
22 Young JZ. Philosophy and the brain. New Yok, NY, US Oxford University Press 1987, viii 233 pp.
23 Lloyd-Jones DM. Truth Unchanged Unchanging. Crossway Books March 31 1993. ISBN-10 0-89107-706-5 www.crossway.org Foreword www.truthforlife.org>fore>Alistair Begg ..
24 Murray Iain (2013). Life of Martyn Lloyd-Jones 1899-1980 Banner of Truth Trust Edinburgh. [This doctor qualified from St Bartholomew’s Hospital London University with First Class Honours and Distinction in Medicine & Therapeutics. Proceeded Doctorate in Medicine with his MD Thesis on Subacute Bacterial Endocarditis. Assisted Lord Horder, Physician to King George V, then suddenly announced retirement from Clinical Medicine and became a preacher. Those not allergic to Christian Worship may wish to listen to Dr Martyn Lloyd-Jones MD MRCP. Listen to one of his messages at Westminster Chapel on 24th November 1963, Sunday after assassination of President Kennedy: Go to www.soundcloud.com/dawid1 and click on JFK. I was there that never to be forgotten Sunday evening. Christians will cherish Dr Martyn Lloyd-Jones’ 15-minute-long extempore prayer after the second hymn, plus his never to be forgotten long sermon after the 3rd hymn “In the cross of Christ I glory”. When he stepped down from the pulpit drenched in sweat, having expounded Galatians 6 verse 14, and after the last hymn “Abide with me” and Benediction, we just sat there, stunned!] Dr Martyn Lloyd-Jones preached more than 1600 sermons. Jonathan Catherwood has all the details – jonathan@mljtrust.org
25 Konotey-Ahulu FID. The spiritual and the psychological in Clinical Medicine. (Personal View) BMJ 1977; 1: 1595 www.bmj.com/cgi/reprint/1/6076/1595.pdf doi:10.1136/6076/1595 June 15.
26 Lloyd-Jones DM. Spiritual Depression: Its Causes and Cure. (ISBN 9780802813879) Amazon’s Book Store www.amazon.co.uk>Spiritual-De [One of top 100 Millennium books]
27 Lloyd-Jones DM. Conversions Psychological & Spiritual https://www.amazon.co.uk>Co 9780851100098 December 1 1959. Critique of Dr William Sargant’s Battle for the Mind
28 Konotey-Ahulu Felix & Rosemary – 50 Years.mov – YouTube https://www.youtube.com 50th Wedding Anniversary [Dr Martyn Lloyd-Jones marries them Easter Monday April 23 1962]
29 Konotey-Ahulu FID. Sickle Cell Trait: As with Statins When leading editors disagree please give principles same weight as details – September 2016 http://www.sicklecel.md/blog/index.php/2016/09/statins-when-leadingl-editors-disagree-please-give-principles-same-weight-as-details/
30 Laine C. Scientific misconduct hurts. Ann Intern Med 2016. doi:10.7326/M16-2550. pmid:27951591.
31 Dyer O. Peer reviewer stole article and published it as his own. BMJ 2016; 355:i6768. doi:10.1136/bmj.i6768. 3
32 Huang Wel. Peer reviewer stole article and published it as its own BMJ 2016; 355:i6768 doi:10.1136/bmj.i6768 :
33 Konotey-Ahulu FID. Born on a Saturday? Science vs History On The Origin and End of the World. Creation 38(4):2016 CREATION.com
34 Konotey-Ahulu FID. Case of lightning burns. BMJ 1963; 1: 1547. June 8. doi:10.1136/bmj. 1.5344.1547 http://www.bmj.com/cgi/reprint/1/5344/1547.apdf
35 Konotey-Ahulu FID. Superstition and phenomena in Africa Personal View. BMJ 1969; 2:48 http://www.bmj.com/cgi/reprint/3/5664/235.pdf doi:10.1136/bmj.2.5648.48 April 15
36 Konotey-Ahulu FID. The supra-scientific in clinical medicine: a challenge to Professor Know-All. doi:10.1136/bmj.323.7327.1452 Brit Med J 2001; 323(7327): 1452-1453 (22-29 Dec) http://www.bmj.com/cgi/reprint/323/7327/1452.pdf
37 Konotey-Ahulu FID. History versus Limits of Science: Is Solomonic Genius a Y Chromosome Phenomenon? J Genet Disorders Genetic Reports 2014; 3: 2
http://bit.ly/1wyq5H5 [Quoted Konotey-Ahulu FID (2012) “Private Thoughts: There is no evidence that I was born on a Saturday. Postgraduate Medical Journal of Ghana 1: 32-33 33” which often proved superiority of history over science in arriving at truth].
38 Konotey-Ahulu FID. MILLENNIUM Hymn – TIME WAS CREATED. http://bit.ly/cRrZ0s 2000 http://www.youtube.com/watch?v=4hconD91uNs .(Seven verses with Music)
39 Holy Bible: St John chapter 8 verse 58 – JESUS said to them “Most assuredly, I say to you: before Abraham was, I AM”.